Biblio du mois : Avril 2018
Les beaux jours ne font que commencer mais voilà qu’arrive la nouvelle biblio du mois !
On vous a laissé le temps de faire une bonne rentrée mais il est temps maintenant d’attaquer un peu de biblio pour faire la discussion en stage 😉
Pour cela, l’AJAR Paris reste à vos côtés !
Au programme, ce mois-ci, on parle d’ALR avec (PECs I and PECs II) en chirurgie du sein ou du JAMA qui se met aux intubations de nouveaux-nés ou des Mises au point sur la gestion péri-opératoire des patients sous AOD ou avec un QT long ?
A part cela, tous les domaines seront abordés ce mois-ci avec notamment le surprenant Retrait des recommandations sur l’AVC de l’AHA/ACC que vous avez pu lire sur nos précédentes biblios (https://www.ajar-online.fr/biblio-du-mois-janvier-2018/).
Pour finir des études intéressantes sur les éléments de la NFS, les détails comptent 😉
Pour la traduction de notre biblio, trouver vos articles ou encore mieux suivre la biblio du mois… voici nos astuces :
https://www.ajar-online.fr/biblio-du-mois-le-tuto-pour-se-maintenir-informe/
Intubation néo-natale avec Atropine + Propofol versus Atropine + Atracurium + Sufentanil ?
Durrmeyer et al., JAMA 2018
https://jamanetwork.com/journals/jama/article-abstract/2679941?redirect=true
Importance Propofol or a combination of a synthetic opioid and muscle relaxant are both recommended for premedication before neonatal intubation but have yet to be compared.
Objective To compare prolonged desaturation during neonatal nasotracheal intubation after premedication with atropine-propofol vs atropine-atracurium-sufentanil treatment.
Design, Setting, and Participants Multicenter, double-blind, randomized clinical trial (2012-2016) in 6 NICUs in France that included 173 neonates requiring nonemergency intubation. The study was interrupted due to expired study kits and lack of funding.
Interventions Eighty-nine participants were randomly assigned to the atropine-propofol group and 82 to the atropine-atracurium-sufentanil group before nasotracheal intubation.
Main Outcomes and Measures The primary outcome was prolonged desaturation (Spo2 <80% lasting > 60 seconds), using intention-to-treat analysis using mixed models. Secondary outcomes assessed the characteristics of the procedure and its tolerance.
Results Of 173 neonates randomized (mean gestational age, 30.6 weeks; mean birth weight, 1502 g; 71 girls), 171 (99%) completed the trial. Of 89 infants, 53 (59.6%) in the atropine-propofol group vs 54 of 82 (65.9%) in the atropine-atracurium-sufentanil group achieved the primary outcome (adjusted RD, −6.4; 95% CI, −21.0 to 8.1; P = .38). The atropine-propofol group had a longer mean procedure duration than did the atropine-atracurium-sufentanil group (adjusted RD, 1.7 minutes; 95% CI, 0.1-3.3 minutes; P = .04); a less frequent excellent quality of sedation rate, 51.7% (45 of 87) vs 92.6% (75 of 81; P < .001); a shorter median time to respiratory recovery, 14 minutes (IQR, 8-34 minutes) vs 33 minutes (IQR, 15-56 minutes; P = .002), and shorter median time to limb movement recovery, 18 minutes (IQR, 10-43 minutes) vs 36 minutes (IQR, 19-65 minutes; P = .003). In the 60 minutes after inclusion, Spo2 was preserved significantly better in the atropine-propofol group (time × treatment interaction P = .02). Of the atropine-propofol group 20.6% had head ultrasound scans that showed worsening intracranial hemorrhaging (any or increased intraventricular hemorrhage) in the 7 days after randomization vs 17.6% in the atropine-atracurium-sufentanil group (adjusted RD, 1.2; 95% CI, −13.1 to 15.5, P = .87). Severe adverse events occurred in 11% of the atropine-propofol group and in 20% of the atropine-atracurium-sufentanil group.
Conclusions and Relevance Among neonates undergoing nonemergency nasotracheal intubation, the frequency of prolonged desaturation did not differ significantly between atropine used with propofol or atropine used with atracurium and sufentanil. However, the study may have been underpowered to detect a clinically important difference, and further research may be warranted.
L’HTAP chez un insuffisant cardiaque à FEVG conservé : facteur de surmortalité ?
Importance Heart failure with preserved ejection fraction (HFpEF) is highly prevalent, yet there are no specific therapies, possibly due to phenotypic heterogeneity. The development of pulmonary hypertension (PH) in patients with HFpEF is considered a high-risk phenotype in need of targeted therapies, but there have been limited hemodynamic and outcomes data.
Objective To identify the hemodynamic characteristics and outcomes of PH-HFpEF.
Design, Setting, and Participants Cohort study of participants who had a right heart catheterization from January 2005 to September 2012 (median [interquartile range] follow-up time, 1578 [554-2513] days) were analyzed. Hemodynamic catheterization data was linked to the clinical data repository of all inpatient and outpatient encounters across a health system. Single tertiary referral center for heart failure and PH within a large health care network using a common clinical data repository was studied. There were 19 262 procedures in 10 023 participants.
Exposures Participants were classified as having no PH, precapillary PH, or PH in the setting of left heart disease (reduced or preserved ejection fraction). Pulmonary hypertension associated with HFpEF was defined as mean pulmonary artery pressure of 25 mm Hg or more, pulmonary artery wedge pressure of 15 mm Hg or more, and left ventricular ejection fraction of 45% or more. Pulmonary hypertension severity was quantified by the hemodynamic parameters transpulmonary gradient, pulmonary vascular resistance, and diastolic pulmonary gradient.
Main Outcomes and Measures The primary outcome was time to all-cause mortality. Secondary outcomes were time to acute hospitalization and cardiovascular hospitalization.
Results The mean (SD) of all study individuals was 65 (38) years. Of 10 023 individuals, 2587 (25.8%) had PH-HFpEF. Mortality was 23.6% at 1 year and 48.2% at 5 years. Cardiac hospitalizations occurred in 28.1% at 1 year and 47.4% at 5 years. The frequency of precapillary PH using clinically defined cut-offs for transpulmonary gradient (>12 mm Hg), pulmonary vascular resistance (3 Woods units), and diastolic pulmonary gradient (≥7 mm Hg) were 12.6%, 8.8%, and 3.5%, respectively. Transpulmonary gradient, pulmonary vascular resistance, and diastolic pressure gradient were predictive of mortality and cardiac hospitalizations.
Conclusions and Relevance In a large cohort referred for invasive hemodynamic assessment, PH-HFpEF was common. Transpulmonary gradient, pulmonary vascular resistance, and diastolic pulmonary gradient are all associated with mortality and cardiac hospitalizations.
PAS < 120mmHg chez un insuffisant cardiaque à FEVG conservé : facteur de surmortalité ?
https://jamanetwork.com/journals/jamacardiology/article-abstract/2672572?redirect=true
doi:10.1001/jamacardio.2017.5365
Importance Lower systolic blood pressure (SBP) levels are associated with poor outcomes in patients with heart failure. Less is known about this association in heart failure with preserved ejection fraction (HFpEF).
Objective To determine the associations of SBP levels with mortality and other outcomes in HFpEF.
Design, Setting, and Participants A propensity score–matched observational study of the Medicare-linked Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients with Heart Failure (OPTIMIZE-HF) registry included 25 354 patients who were discharged alive; 8873 (35.0%) had an ejection fraction of at least 50%, and of these, 3915 (44.1%) had stable SBP levels (≤20 mm Hg admission to discharge variation). Data were collected from 259 hospitals in 48 states between March 1, 2003, and December 31, 2004. Data were analyzed from March 1, 2003, to December 31, 2008.
Exposure Discharge SBP levels less than 120 mm Hg. A total of 1076 of 3915 (27.5%) had SBP levels less than 120 mm Hg, of whom 901 (83.7%) were matched by propensity scores with 901 patients with SBP levels of 120 mm Hg or greater who were balanced on 58 baseline characteristics.
Main Outcomes and Measures Thirty-day, 1-year, and overall all-cause mortality and heart failure readmission through December 31, 2008.
Results The 1802 matched patients had a mean (SD) age of 79 (10) years; 1147 (63.7%) were women, and 134 (7.4%) were African American. Thirty-day all-cause mortality occurred in 91 (10%) and 45 (5%) of matched patients with discharge SBP of less than 120 mm Hg vs 120 mm Hg or greater, respectively (hazard ratio [HR], 2.07; 95% CI, 1.45-2.95; P < .001). Systolic blood pressure level less than 120 mm Hg was also associated with a higher risk of mortality at 1 year (39% vs 31%; HR, 1.36; 95% CI, 1.16-1.59; P < .001) and during a median follow-up of 2.1 (overall 6) years (HR, 1.17; 95% CI, 1.05-1.30; P = .005). Systolic blood pressure level less than 120 mm Hg was associated with a higher risk of heart failure readmission at 30 days (HR, 1.47; 95% CI, 1.08-2.01; P = .02) but not at 1 or 6 years. Hazard ratios for the combined end point of heart failure readmission or all-cause mortality associated with SBP level less than 120 mm at 30 days, 1 year, and overall were 1.71 (95% CI, 1.34-2.18; P < .001), 1.21 (95% CI, 1.07-1.38; P = .004), and 1.12 (95% CI, 1.01-1.24; P = .03), respectively.
Conclusions and Relevance Among hospitalized patients with HFpEF, an SBP level less than 120 mm Hg is significantly associated with poor outcomes. Future studies need to prospectively evaluate optimal SBP treatment goals in patients with HFpEF.
Revue sur le syndrome de sevrage néo-natal
Wachman et al., JAMA, 2018
https://jamanetwork.com/journals/jama/article-abstract/2677452?redirect=true
doi:10.1001/jama.2018.2640
Revue sur taille des végétations et risque embolique
Mohananey et al.,
https://jamanetwork.com/journals/jamainternalmedicine/article-abstract/2672577?redirect=true
Une revue pour (enfin) comprendre le base excess
Méta-analyse : L’excès d’oxygène tue
Global Health : Revue des outcomes en péri-opératoire en Afrique
Petites doses de Dexmedetomidine contre le Delirium ?
https://www.atsjournals.org/doi/abs/10.1164/rccm.201710-1995OC
https://doi.org/10.1164/rccm.201710-1995OC
Rationale: Dexmedetomidine is associated with less delirium than benzodiazepines and better sleep architecture than either benzodiazepines or propofol; its effect on delirium and sleep when administered at night to patients requiring sedation remains unclear.
Objectives: To determine if nocturnal dexmedetomidine prevents delirium and improves sleep in critically ill adults.
Methods: This two-center, double-blind, placebo-controlled trial randomized 100 delirium-free critically ill adults receiving sedatives to receive nocturnal (9:30 p.m. to 6:15 a.m.) intravenous dexmedetomidine (0.2 μg/kg/h, titrated by 0.1 μg /kg/h every 15 min until a goal Richmond Agitation and Sedation Scale score of −1 or maximum rate of 0.7 μg/kg/h was reached) or placebo until ICU discharge. During study infusions, all sedatives were halved; opioids were unchanged. Delirium was assessed using the Intensive Care Delirium Screening Checklist every 12 hours throughout the ICU admission. Sleep was evaluated each morning by the Leeds Sleep Evaluation Questionnaire.
Measurements and Main Results: Nocturnal dexmedetomidine (vs. placebo) was associated with a greater proportion of patients who remained delirium-free during the ICU stay (dexmedetomidine [40 (80%) of 50 patients] vs. placebo [27 (54%) of 50 patients]; relative risk, 0.44; 95% confidence interval, 0.23–0.82; P = 0.006). The average Leeds Sleep Evaluation Questionnaire score was similar (mean difference, 0.02; 95% confidence interval, 0.42–1.92) between the 34 dexmedetomidine (average seven assessments per patient) and 30 placebo (six per patient) group patients able to provide one or more assessments. Incidence of hypotension, bradycardia, or both did not differ significantly between groups.
Conclusions: Nocturnal administration of low-dose dexmedetomidine in critically ill adults reduces the incidence of delirium during the ICU stay; patient-reported sleep quality appears unchanged.
Exploration pulmonaire non invasive dans le SDRA grâce aux filtres échangeurs de chaleur et d’humidité ?
https://www.atsjournals.org/doi/full/10.1164/rccm.201707-1474OC
https://doi.org/10.1164/rccm.201707-1474OC
Rationale: A major barrier to a more complete understanding of acute respiratory distress syndrome (ARDS) pathophysiology is the inability to sample the distal airspace of patients with ARDS. The heat moisture exchanger (HME) filter is an inline bacteriostatic sponge that collects exhaled moisture from the lungs of mechanically ventilated patients.
Objectives: To test the hypothesis that HME filter fluid (HMEF) represents the distal airspace fluid in patients with ARDS.
Methods: Samples of HMEF were collected from 37 patients with acute pulmonary edema (either from ARDS or hydrostatic causes [HYDRO; control subjects]). Concurrent undiluted pulmonary edema fluid (EF) and HMEF were collected from six patients. HMEF from 11 patients (8 ARDS and 3 HYDRO) were analyzed by liquid chromatography–coupled tandem mass spectometry. Total protein (bicinchoninic acid assay), MMP-9 (matrix metalloproteinase-9), and MPO (myeloperoxidase) (ELISA) were measured in 29 subjects with ARDS and 5 subjects with HYDRO. SP-D (surfactant protein-D), RAGE (receptor for advanced glycation end-products) (ELISA), and cytokines (IL-1β, IL-6, IL-8, and tumor necrosis factor-α) (electrochemiluminescent assays) were measured in six concurrent HMEF and EF samples.
Measurements and Main Results: Liquid chromatography–coupled tandem mass spectrometry on concurrent EF and HMEF samples from four patients revealed similar base peak intensities and m/z values indicating similar protein composition. There were 21 significantly elevated proteins in HMEF from patients with ARDS versus HYDRO. Eight proteins measured in concurrent EF and HMEF from six patients were highly correlated. In HMEF, total protein and MMP-9 were significantly higher in ARDS than in HYDRO.
Conclusions: These data suggest that HMEF is a novel, noninvasive method to accurately sample the distal airspace in patients with ARDS.
Keywords: acute respiratory distress syndrome; airspace fluid; biomarkers; heat moisture exchanger filter; pulmonary edema fluid
Cistracrium vs Vecuronium dans le SDRA : le Cisatracrium conserve sa place de curare de première intention
Sottile et al., AJRCCM, 2018
https://www.atsjournals.org/doi/full/10.1164/rccm.201706-1132OC
https://doi.org/10.1164/rccm.201706-1132OC
Rationale: The neuromuscular blocking agent cisatracurium may improve mortality for patients with moderate-to-severe acute respiratory distress syndrome (ARDS). Other neuromuscular blocking agents, such as vecuronium, are commonly used and have different mechanisms of action, side effects, cost, and availability in the setting of drug shortages.
Objectives: To determine whether cisatracurium is associated with improved outcomes when compared with vecuronium in patients at risk for and with ARDS.
Methods: Using a nationally representative database, patients who were admitted to the ICU with a diagnosis of ARDS or an ARDS risk factor, received mechanical ventilation, and were treated with a continuous infusion of neuromuscular blocking agent for at least 2 days within 2 days of hospital admission were included. Patients were stratified into two groups: those who received cisatracurium or vecuronium. Propensity matching was used to balance both patient- and hospital-specific factors. Outcomes included hospital mortality, duration of mechanical ventilation, ICU and hospital duration, and discharge location.
Measurements and Main Results: Propensity matching successfully balanced all covariates for 3,802 patients (1,901 per group). There was no significant difference in mortality (odds ratio, 0.932; P = 0.40) or hospital days (–0.66 d; P = 0.411) between groups. However, patients treated with cisatracurium had fewer ventilator days (–1.01 d; P = 0.005) and ICU days (–0.98 d; P = 0.028) but were equally likely to be discharged home (odds ratio, 1.19; P = 0.056).
Conclusions: When compared with vecuronium, cisatracurium was not associated with a difference in mortality but was associated with improvements in other clinically important outcomes. These data suggest that cisatracurium may be the preferred neuromuscular blocking agent for patients at risk for and with ARDS.
L’apnée du sommeil facteur de risque de maladie d’Alzheimer ?
https://doi.org/10.1164/rccm.201704-0704OC
Plus grande morbidité post-opératoire dans la césarienne programmée avec AG vs ALR ?
Abe et al., BJA, 2018
https://bjanaesthesia.org/article/S0007-0912(17)54186-0/fulltext
Background
Although the incidence of maternal mortality during Caesarean delivery remains very low, the rate of severe maternal morbidity is increasing. Improvements in obstetric anaesthetic practice have resulted in a dramatic reduction in the risk of maternal death from general anaesthesia. Less clear is whether the risk of severe maternal morbidity differs according to mode of anaesthesia for women undergoing Caesarean delivery. We analysed the association between the mode of anaesthesia and severe maternal morbidity during Caesarean delivery using a nationally representative inpatient database.
Methods
We identified 89 225 women undergoing scheduled Caesarean delivery from the Diagnosis Procedure Combination database in Japan, 2010–2013. We defined severe maternal morbidity as the presence of any life-threatening complications and identified women with severe maternal morbidity from the database. Propensity score-matched analysis was carried out to compare the odds of severe maternal morbidity between women who underwent general vs neuraxial anaesthesia.
Results
Of 89 225 women, 10 058 received general anaesthesia and 79 167 received neuraxial anaesthesia. In the propensity score-matched analysis with 10 046 pairs, a higher incidence of severe maternal morbidity was observed among patients receiving general (2.00%) rather than neuraxial anaesthesia (0.76%). The odds ratio of severe maternal morbidity was 2.68 (95% CI, 1.97–3.64) among women receiving general compared with neuraxial anaesthesia.
Conclusions
For scheduled Caesarean delivery, general anaesthesia compared with neuraxial anaesthesia is associated with greater odds for severe maternal morbidity. However, we should be cautious with interpretation of these findings because they may be explained by confounding indications.
Stratégie de gestion hémodynamique sous guidage du doppler œsophagien (étude FEDORA)
Calvo-Vecino et al., BJA, 2018
https://bjanaesthesia.org/article/S0007-0912(17)54207-5/fulltext
Background
The aim of this study was to evaluate postoperative complications in patients having major elective surgery using oesophageal Doppler monitor-guided goal-directed haemodynamic therapy (GDHT), in which administration of fluids, inotropes, and vasopressors was guided by stroke volume, mean arterial pressure, and cardiac index.
Methods
The FEDORA trial was a prospective, multicentre, randomised, parallel-group, controlled patient- and observer-blind trial conducted in adults scheduled for major elective surgery. Randomization and allocation were carried out by a central computer system. In the control group, intraoperative fluids were given based on traditional principles. In the GDHT group, the intraoperative goals were to maintain a maximal stroke volume, with mean arterial pressure >70 mm Hg, and cardiac index ≥2.5 litres min−1 m−2. The primary outcome was percentage of patients with moderate or severe postoperative complications during the first 180 days after surgery.
Results
In total, 450 patients were randomized to the GDHT group (n=224) or control group (n=226). Data from 420 subjects were analysed. There were significantly fewer with complications in the GDHT group (8.6% vs 16.6%, P=0.018). There were also fewer complications (acute kidney disease, pulmonary oedema, respiratory distress syndrome, wound infections, etc.), and length of hospital stay was shorter in the GDHT group. There was no significant difference in mortality between groups.
Conclusions
Oesophageal Doppler monitor-guided GDHT reduced postoperative complications and hospital length of stay in low–moderate risk patients undergoing intermediate risk surgery, with no difference in mortality at 180 days.
Cathéter péri-nerveux vs single shot dans la chirurgie du sein
O’Scanaill et al., BJA, 2018
https://bjanaesthesia.org/article/S0007-0912(18)30030-8/fulltext
Background
Pectoral plane blocks (PECs) are increasingly used in analgesia for patients undergoing breast surgery, and were recently found to be at least equivalent to single-shot paravertebral anaesthesia. However, there are no data comparing PECs with the popular practice of continuous local anaesthetic wound infusion (LA infusion) analgesia for breast surgery. Therefore, we compared the efficacy and safety of PECs blocks with LA infusion, or a combination of both in patients undergoing non-ambulatory breast-cancer surgery.
Methods
This single-centre, prospective, randomised, double-blind trial analysed 45 women to receive either PECs blocks [levobupivacaine 0.25%, 10 ml PECs I and levobupivacaine 0.25%, 20 ml PECs II (PECs group); LA infusion catheter (levobupivacaine 0.1% at 10 ml h−1 for 24 h (LA infusion group); or both (PECs and LA infusion)]. The primary outcome measure was area under the curve of the pain verbal rating score whilst moving vs time (AUC) over 24 h. Secondary outcomes included total opioid consumption at 24 h.
Results
AUC moving was mean (SD) 71 (34) mm h−1vs 58 (41) vs 23 (20) in PECs, LA infusion, and both, respectively; P=0.002. AUC at rest was also significantly lower in patients receiving both. The total 24 h opioid consumption [median (25–75%)] was 14 mg (9–26) vs 11 (8–24) vs 9 (5–11); P=0.4. No adverse events were observed.
Conclusions
The combination of both pre-incisional PECs blocks and postoperative LA infusion provides better analgesia over 24 h than either technique alone after non-ambulatory breast-cancer surgery.
Mises au point :
– sur la gestion péri-opératoire des patients avec un syndrome du QT long
O’Hare et al., BJA, 2018
https://bjanaesthesia.org/article/S0007-0912(18)30037-0/fulltext
– sur la prise en charge des patients sous anticoagulants oraux directs en cas de chirurgie non programmée
Eikelboom et al., BJA, 2018
https://bjanaesthesia.org/article/S0007-0912(17)54077-5/fulltext
Les réponses en 10 questions !
La mesure de la PVC peut-elle aider :
– à guider l’expansion volémique ?
Daniel De Backer et Jean-Louis Vincent, Critical Care, 2018
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-1959-3
Abstract
The central venous pressure (CVP) is the most frequently used variable to guide fluid resuscitation in critically ill patients, although its use has been challenged. In this viewpoint, we use a question and answer format to highlight the potential advantages and limitations of using CVP measurements to guide fluid resuscitation.
– …ou la déplétion ?
Legrand M et al, Critical Care, 2018
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2016-y
Faut-il évoquer précocement une maladie de Still devant des défaillances d’organes fébriles inexpliquées ?
Selon cette revue, Oui : Dosez la ferritine !
Néel A et al, Critical Care, 2018
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2012-2
BACKGROUND:
Adult-onset Still disease (AOSD) is a rare systemic inflammatory disorder. A few patients develop organ complications that can be life-threatening. Our objectives were to describe the disease course and phenotype of life-threatening AOSD, including response to therapy and long-term outcome.
METHODS:
A multicenter case series of intensive care medicine (ICU) patients with life-threatening AOSD and a systematic literature review.
RESULTS:
Twenty patients were included. ICU admission mostly occurred at disease onset (90%). Disease manifestations included fever (100%), sore throat (65%), skin rash (65%), and arthromyalgia (55%). Serum ferritin was markedly high (median: 29,110 ng/mL). Acute respiratory failure, shock and multiple organ failure occurred in 15 (75%), 10 (50%), and 7 (35%) cases, respectively. Hemophagocytosis was demonstrated in eight cases. Two patients died. Treatment delay was significant. All patients received corticosteroids. Response rate was 50%. As second-line, intravenous immunoglobulins were ineffective. Anakinra was highly effective. After ICU discharge, most patients required additional treatment. Literature analysis included 79 cases of AOSD with organ manifestations, which mainly included reactive hemophagocytic syndrome (42%), acute respiratory failure (34%), and cardiac complications (23%). Response rate to corticosteroids was 68%. Response rates to IVIgs, cyclosporin, and anakinra were 50%, 80%, and 100%, respectively.
CONCLUSIONS:
AOSD should be recognized as a rare cause of sepsis mimic in patients with fever of unknown origin admitted to the ICU. The diagnosis relies on a few simple clinical clues. Early intensive treatment may be discussed. IVIgs should be abandoned. Long-term prognosis is favorable.
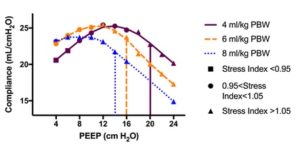
La meilleure PEP dépend du volume courant !
McKown, Critical Care 2018
https://ccforum.biomedcentral.com/articles/10.1186/s13054-018-2047-4
https://doi.org/10.1186/s13054-018-2047-4
Induction IV versus inhalatoire chez les enfants à risque de complications respiratoires
Ramgolam et al., Anesthesiology, 2018
https://insights.ovid.com/crossref?an=00000542-900000000-96939
DOI: 10.1097/ALN.0000000000002152
Background:
Limited evidence suggests that children have a lower incidence of perioperative respiratory adverse events when intravenous propofol is used compared with inhalational sevoflurane for the anesthesia induction. Limiting these events can improve recovery time as well as decreasing surgery waitlists and healthcare costs. This single center open-label randomized controlled trial assessed the impact of the anesthesia induction technique on the occurrence of perioperative respiratory adverse events in children at high risk of those events.
Methods:
Children (N = 300; 0 to 8 yr) with at least two clinically relevant risk factors for perioperative respiratory adverse events and deemed suitable for either technique of anesthesia induction were recruited and randomized to either intravenous propofol or inhalational sevoflurane. The primary outcome was the difference in the rate of occurrence of perioperative respiratory adverse events between children receiving intravenous induction and those receiving inhalation induction of anesthesia.
Results:
Children receiving intravenous propofol were significantly less likely to experience perioperative respiratory adverse events compared with those who received inhalational sevoflurane after adjusting for age, sex, American Society of Anesthesiologists physical status and weight (perioperative respiratory adverse event: 39/149 [26%] vs. 64/149 [43%], relative risk [RR]: 1.7, 95% CI: 1.2 to 2.3, P = 0.002, respiratory adverse events at induction: 16/149 [11%] vs. 47/149 [32%], RR: 3.06, 95% CI: 1.8 to 5.2, P < 0.001).
Conclusions:
Where clinically appropriate, anesthesiologists should consider using an intravenous propofol induction technique in children who are at high risk of experiencing perioperative respiratory adverse events.
La PCT inutile pour guider l’antibiothérapie lors d’une exacerbation aiguë de BPCO ?
Daubin et al., ICM, 2018
Purpose
To compare the efficacy of an antibiotic protocol guided by serum procalcitonin (PCT) with that of standard antibiotic therapy in severe acute exacerbations of COPD (AECOPDs) admitted to the intensive care unit (ICU).
Methods
We conducted a multicenter, randomized trial in France. Patients experiencing severe AECOPDs were assigned to groups whose antibiotic therapy was guided by (1) a 5-day PCT algorithm with predefined cutoff values for the initiation or stoppage of antibiotics (PCT group) or (2) standard guidelines (control group). The primary endpoint was 3-month mortality. The predefined noninferiority margin was 12%.
Results
A total of 302 patients were randomized into the PCT (n = 151) and control (n = 151) groups. Thirty patients (20%) in the PCT group and 21 patients (14%) in the control group died within 3 months of admission (adjusted difference, 6.6%; 90% CI − 0.3 to 13.5%). Among patients without antibiotic therapy at baseline (n = 119), the use of PCT significantly increased 3-month mortality [19/61 (31%) vs. 7/58 (12%), p = 0.015]. The in-ICU and in-hospital antibiotic exposure durations, were similar between the PCT and control group (5.2 ± 6.5 days in the PCT group vs. 5.4 ± 4.4 days in the control group, p = 0.85 and 7.9 ± 8 days in the PCT group vs. 7.7 ± 5.7 days in the control group, p = 0.75, respectively).
Conclusion
The PCT group failed to demonstrate non-inferiority with respect to 3-month mortality and failed to reduce in-ICU and in-hospital antibiotic exposure in AECOPDs admitted to the ICU.
Revue sur le traitement des anémies hémolytiques
Boutboul et al., ICM, 2018
Consommation d’opioïdes avant admission en réa : surmortalité ?
Munch et al., CCM, 2018
https://insights.ovid.com/pubmed?pmid=29528945
DOI: 10.1097/CCM.0000000000003080
Objectives:
Compare all-cause mortality following nonsurgical ICU admission for opioid users with nonusers.
Design:
Nationwide register-based cohort study.
Setting:
All 43 ICUs in Denmark (7,028,668 citizens cumulatively during the study period). The Danish National Health Service provides universal healthcare, guaranteeing equal access to healthcare along with partial reimbursement for prescribed drugs.
Patients:
All 118,388 nonsurgical patients admitted to an ICU from 2005 to 2014.
Intervention:
Patients were categorized according to timing of last redeemed opioid prescription before admission: current user (prior 0–30 d), recent user (prior 31–365 d), former user (prior 365+ d), or nonuser (no prescription since 1994).
Measurements:
All-cause mortality 0–30 days and 31–365 days following ICU admission was calculated using the Kaplan-Meier method. Crude and adjusted hazard ratios with 95% CIs were computed using Cox regression, comparing users with nonusers. Adjusted models included age, gender, socioeconomic factors, comedications, and comorbidity.
Main Results:
Fifteen percent of the patients were current opioid users, 15% recent users, 30% former users, and 40% nonusers. Zero- to 30-day mortality was 35% for current users, 29% for recent users, 24% for former users, and 21% for nonusers. After confounder adjustment, current users remained at elevated risk during the first 30 days following ICU admission (hazard ratio, 1.20; 95% CI, 1.15–1.24). No association remained for recent or former users. A similar pattern was evident for 31–365-day all-cause mortality: 24% for current users, 19% for recent users, 13% for former users, and 10% for nonusers. During 31–365 days of follow-up, both current users and recent users remained at elevated risk of mortality after adjustment (hazard ratio, 1.47; 95% CI, 1.39–1.55 and hazard ratio, 1.20; 95% CI, 1.13–1.27, respectively).
Conclusions:
Current opioid users experience increased mortality during the first year following ICU admission.
Hyperoxie : aggravation de la morbi-mortalité dans le SDRA
Aggarwal et al., CCM, 2018
https://journals.lww.com/ccmjournal/Abstract/2018/04000/Oxygen_Exposure_Resulting_in_Arterial_Oxygen.6.aspx
doi: 10.1097/CCM.0000000000002886
Objectives:
High fractions of inspired oxygen may augment lung damage to exacerbate lung injury in patients with acute respiratory distress syndrome. Participants enrolled in Acute Respiratory Distress Syndrome Network trials had a goal partial pressure of oxygen in arterial blood range of 55–80 mm Hg, yet the effect of oxygen exposure above this arterial oxygen tension range on clinical outcomes is unknown. We sought to determine if oxygen exposure that resulted in a partial pressure of oxygen in arterial blood above goal (> 80 mm Hg) was associated with worse outcomes in patients with acute respiratory distress syndrome.
Design:
Longitudinal analysis of data collected in these trials.
Setting:
Ten clinical trials conducted at Acute Respiratory Distress Syndrome Network hospitals between 1996 and 2013.
Subjects:
Critically ill patients with acute respiratory distress syndrome.
Measurements and Main Results:
We defined above goal oxygen exposure as the difference between the fraction of inspired oxygen and 0.5 whenever the fraction of inspired oxygen was above 0.5 and when the partial pressure of oxygen in arterial blood was above 80 mm Hg. We then summed above goal oxygen exposures in the first five days to calculate a cumulative above goal oxygen exposure. We determined the effect of a cumulative 5-day above goal oxygen exposure on mortality prior to discharge home at 90 days. Among 2,994 participants (mean age, 51.3 yr; 54% male) with a study-entry partial pressure of oxygen in arterial blood/fraction of inspired oxygen that met acute respiratory distress syndrome criteria, average cumulative above goal oxygen exposure was 0.24 fraction of inspired oxygen-days (interquartile range, 0–0.38). Participants with above goal oxygen exposure were more likely to die (adjusted interquartile range odds ratio, 1.20; 95% CI, 1.11–1.31) and have lower ventilator-free days (adjusted interquartile range mean difference of –0.83; 95% CI, –1.18 to –0.48) and lower hospital-free days (adjusted interquartile range mean difference of –1.38; 95% CI, –2.09 to –0.68). We observed a dose-response relationship between the cumulative above goal oxygen exposure and worsened clinical outcomes for participants with mild, moderate, or severe acute respiratory distress syndrome, suggesting that the observed relationship is not primarily influenced by severity of illness.
Conclusions:
Oxygen exposure resulting in arterial oxygen tensions above the protocol goal occurred frequently and was associated with worse clinical outcomes at all levels of acute respiratory distress syndrome severity.
Diagnostic précoce de SDRA chez les patients sous ventilation non-invasive
Coudroy et al., CCM, 2018
https://journals.lww.com/ccmjournal/Abstract/2018/04000/Early_Identification_of_Acute_Respiratory_Distress.9.aspx
doi: 10.1097/CCM.0000000000002929
Objectives:
To assess whether patients breathing spontaneously under standard oxygen could be recognized early as acute respiratory distress syndrome patients according to the current Berlin definition.
Design:
A post hoc analysis from two prospective studies.
Setting:
Twenty-three French ICUs.
Patients:
All patients admitted for acute hypoxemic respiratory failure and treated with noninvasive ventilation were analyzed. Patients with cardiogenic pulmonary edema, acute exacerbation of chronic obstructive pulmonary disease, or hypercapnia were excluded.
Measurements and Main Results:
The PaO2/FIO2 ratio was estimated at admission under standard oxygen and then under noninvasive ventilation 1 hour after initiation and within the first 24 hours. Among the 219 patients treated with noninvasive ventilation for acute hypoxemic respiratory failure, 180 (82%) had bilateral infiltrates including 161 patients with PaO2/FIO2 less than or equal to 300 mm Hg under standard oxygen. Among them, 127 were treated with positive end-expiratory pressure of at least 5 cm H2O, and 120 (94%) fulfilled criteria for acute respiratory distress syndrome within the first 24 hours. The mortality rate of patients with bilateral infiltrates and PaO2/FIO2 less than or equal to 300 mm Hg under standard oxygen was 29%, a rate very close to that of intubated patients with acute respiratory distress syndrome in the Berlin definition.
Conclusions:
Almost all patients with pulmonary bilateral infiltrates and a PaO2/FIO2 less than or equal to 300 mm Hg under standard oxygen fulfilled the acute respiratory distress syndrome criteria under noninvasive ventilation within the first 24 hours. Their mortality rate was similar to that reported in the Berlin definition of acute respiratory distress syndrome. Therefore, spontaneous breathing patients with the acute respiratory distress syndrome criteria could be identified early without positive pressure ventilation.
La péridurale : moins de mortalité dans la pancréatite aigue ?
et al., CCM, 2018
https://insights.ovid.com/pubmed?pmid=29194144
DOI: 10.1097/CCM.0000000000002874
Objective:
Recent preclinical and clinical data suggest that thoracic epidural analgesia, a technique primarily aimed at decreasing pain, might exert anti-inflammatory effects, enhance splanchnic and pancreatic blood flow during acute pancreatitis; however, the influence of epidural analgesia on mortality remains under investigated in this setting. This study was therefore designed to assess the impact of epidural analgesia on mortality in ICU patients with acute pancreatitis.
Design:
Multicenter retrospective, observational, cohort study.
Setting:
Seventeen French and Belgian ICUs.
Patients:
All patients admitted to with acute pancreatitis between June 2009 and March 2014.
Interventions:
The primary exposure was thoracic epidural analgesia versus standard care without epidural analgesia. The primary outcome was 30-day mortality. Propensity analyses were used to control for bias in treatment assignment and prognostic imbalances.
Measurements and Main Results:
One thousand three ICU patients with acute pancreatitis were enrolled, of whom 212 died within 30 days. Epidural analgesia was used in 46 patients and was associated with reduced mortality in unadjusted analyses (4% vs. 22%; p = 0.003). After adjustment for baseline variables associated with mortality, epidural analgesia was still an independent predictor of 30-day mortality (adjusted odds ratio, 0.10; [95% CI, 0.02–0.49]; p = 0.004). Using propensity score analysis, the risk of all-cause 30-day mortality in patients with acute pancreatitis receiving epidural analgesia was significantly lower than that in matched patients who did not receive epidural analgesia (2% vs. 17%; p = 0.01).
Conclusions:
Among critically ill patients with acute pancreatitis, mortality at 30 days was lower in patients who received epidural analgesia than in comparable patients who did not. These findings support ongoing research on the use of epidural analgesia as a therapeutic intervention in acute pancreatitis.
Retrait des recommendations ACC/AHA sur la prise en charge de l’AVC
http://stroke.ahajournals.org/content/early/2018/04/17/STR.0000000000000172
https://doi.org/10.1161/STR.0000000000000172
Hyperoxie à la phase précoce post-ACR : moins bon pronostic neurologique
Roberts et al., Circulation, 2018
http://circ.ahajournals.org/content/early/2018/01/25/CIRCULATIONAHA.117.032054
https://doi.org/10.1161/CIRCULATIONAHA.117.032054
Background—Studies examining the association between hyperoxia exposure after resuscitation from cardiac arrest and clinical outcomes have reported conflicting results. Our objective was to test the hypothesis that early post-resuscitation hyperoxia is associated with poor neurological outcome.
Methods—Multi-center, prospective cohort study. We included adult, cardiac arrest patients who were mechanically ventilated and received targeted temperature management after return of spontaneous circulation (ROSC). We excluded patients with cardiac arrest due to trauma or sepsis. Per protocol, partial pressure of arterial oxygen (PaO2) was measured at one and six hours after ROSC. Hyperoxia was defined as a PaO2 > 300 mmHg during the initial six hours after ROSC. The primary outcome was poor neurological function at hospital discharge, defined as a modified Rankin Scale > 3. Multivariable generalized linear regression with a log link was used to test the association between PaO2 and poor neurological outcome. To assess if there was an association between other supranormal PaO2 levels and poor neurological outcome, we used other PaO2 cut points to define hyperoxia (i.e. 100, 150, 200, 250, 350, 400 mmHg).
Results—Of the 280 patients included, 105 (38%) had exposure to hyperoxia. Poor neurological function at hospital discharge occurred in 70% of patients in the entire cohort, and 77% vs. 65% among patients with and without exposure to hyperoxia respectively [absolute risk difference 12% (95% CI 1% – 23%)]. Hyperoxia was independently associated with poor neurological function, relative risk 1.23 (95% CI 1.11 – 1.35). On multivariable analysis, a one-hour longer duration of hyperoxia exposure was associated with a 3% increase in risk of poor neurological outcome [relative risk 1.03 (95% CI 1.02 – 1.05)]. We found the association with poor neurological outcome began at 300 mmHg or higher.
Conclusions—Early hyperoxia exposure after resuscitation from cardiac arrest was independently associated with poor neurological function at hospital discharge.
Revue sur le rôle des neutrophiles dans le choc septique
Stiel L et al, Shock, 2018
https://journals.lww.com/shockjournal/Abstract/2018/04000/Neutrophil_Activation_During_Septic_Shock.4.aspx
doi: 10.1097/SHK.0000000000000980
In addition to their well-known role as the cellular mediators of immunity, key other roles have been identified for neutrophils during septic shock. Importantly, neutrophils indeed play a critical role in the recently described immunothrombosis concept and in septic shock-induced coagulopathy. Septic shock is one of the most severe forms of infection, characterized by an inadequate host response to the pathogenic organism. This host response involves numerous defense mechanisms with an intense cellular activation, including neutrophil activation. Neutrophils are key cells of innate immunity through complex interactions with vascular cells and their activation may participate in systemic tissue damages. Their activation also leads to the emission of neutrophil extracellular traps, which take part in both pathogen circumscription and phagocytosis, but also in coagulation activation. Neutrophils thus stand at the interface between hemostasis and immunity, called immunothrombosis.
The present review will develop a cellular approach of septic shock pathophysiology focusing on neutrophils as key players of septic shock-induced vascular cell dysfunction and of the host response, associating immunity and hemostasis. We will therefore first develop the role of neutrophils in the interplay between innate and adaptive immunity, and will then highlight recent advances in our understanding of immunothrombosis septic shock-induced coagulopathy.
Le rapport neutrophiles/lymphocytes pour prédire la mortalité dans la décompensation de cirrhose ?
ABSTRACT
These findings suggest that NLR is associated with mortality in ACLF patients admitted to the ICU. Combining NLR, SOFA score, and the need for mechanical ventilation could be a useful prognostic tool to identify ACLF patients at a higher risk of mortality.
Evaluation de la prise en charge conservative de pneumothorax traumatiques
https://journal.chestnet.org/article/S0012-3692(17)32917-3/fulltext
Background
Traumatic pneumothoraces are a common consequence of major trauma. Despite this, there is a paucity of literature regarding their optimal management, including the role of conservative treatment. The aim of this study was to assess the treatment, complications, and outcomes of traumatic pneumothoraces in patients presenting to a major trauma center.
Methods
The prospectively collected Trauma Audit and Research Network (TARN) database was used to identify all patients presenting with traumatic pneumothoraces to a UK major trauma center from April 2012 to December 2016. Demographics, mechanism of injury, injury severity score (ISS), management, and outcomes were analyzed.
Results
Six hundred two patients were included during the study period. Mean age was 48 years (SD, 22 years), and 73% were men. Mean ISS was 26 and inpatient mortality was 9%. Of the 602 traumatic pneumothoraces, 277 of 602 (46%) were initially treated conservatively. Two hundred fifty-two of 277 patients in this cohort (90%) did not require subsequent chest tube insertion, including the majority of patients (56 of 62 [90%]) who were receiving positive pressure ventilation (PPV) on admission. The hazard ratio (HR) for failure of conservative management showed no difference between the ventilated and nonventilated patients (HR, 1.1; P = .84). Only the presence of a large hemothorax was associated with an increased likelihood of failure of conservative management.
Conclusions
In the largest observational study of traumatic pneumothoraces published to date, > 90% of patients whose pneumothorax was managed conservatively never required subsequent tube drainage. Importantly, this also applies to patients requiring PPV, with no significant increased risk of failure of expectant management. These data support a role for conservative management in traumatic pneumothoraces.
Faut-il abandonner le cathéter artériel ?
https://journal.chestnet.org/article/S0012-3692(17)32981-1/fulltext
DOI: https://doi.org/10.1016/j.chest.2017.10.030
Effet protecteur des statines dans le sepsis non lié aux lipides ?
Lee et al., Chest, 2018
https://journal.chestnet.org/article/S0012-3692(17)32803-9/fulltext
Background
Whether statin treatment, proved by recent experimental studies to have an antimicrobial activity, exerts a drug- or a class-specific effect in sepsis remains unknown.
Methods
Short-term mortality in patients with sepsis was analyzed using data from the National Health Insurance Research Database. Use of statins was defined as the cumulative use of a specific statin (atorvastatin, simvastatin, or rosuvastatin) for > 30 days prior to the index sepsis admission. We determined the association between statin and sepsis outcome by multivariate-adjusted Cox models and propensity score (PS)-matched analysis, using a 1:1:1 PS matching technique.
Results
A total of 52,737 patients with sepsis fulfilled the inclusion criteria, of which 1,855 were prescribed atorvastatin, 916 were prescribed simvastatin, and 732 were prescribed rosuvastatin. Compared with nonusers, simvastatin (hazard ratio [HR], 0.72; 95% CI, 0.58-0.90) and atorvastatin (HR, 0.78; 95% CI, 0.68-0.90) were associated with an improved 30-day survival, whereas rosuvastatin was not (HR, 0.87; 95% CI, 0.73-1.04). Using rosuvastatin as the reference, atorvastatin (HR, 0.79; 95% CI, 0.64-0.99) and simvastatin (HR, 0.77; 95% CI, 0.59-0.99) had superior effectiveness in preventing mortality.
Conclusions
Compatible with in vitro experimental findings, our results suggest that the drug-specific effect of statins on sepsis is not correlated to their lipid-lowering potency.
L’évaluation de l’index de collapsibilité de veine cave inférieur par voie sous-costale et trans-hépatique est-elle comparable ?
Shah et al., Chest, 2018
https://journal.chestnet.org/article/S0012-3692(17)32888-X/fulltext
DOI: https://doi.org/10.1016/j.chest.2017.10.002
Background
The collapsibility index of the inferior vena cava is traditionally visualized from the subcostal region in the sagittal plane, referred to here as cIVCSS. Alternatively, the collapsibility index of the inferior vena cava can be visualized from the right midaxillary line in the coronal plane, referred to here as cIVCRC. It is unclear whether values of cIVCRC are comparable with values of cIVCSS because the inferior vena cava collapses asymmetrically into an elliptical form, quantified as the flat ratio of the inferior vena cava (F-IVC). This study aimed (1) to establish if cIVCRC is concordant or discordant to cIVCSS, and (2) to describe how this concordance or discordance is related to F-IVC.
Methods
This single-center cross-sectional study enrolled 110 spontaneously breathing patients. Values of cIVCRC were compared with cIVCSS. Performance of cIVCRC ≥ 42% in predicting fluid responsiveness, defined as cIVCSS ≥ 42%, was assessed. F-IVC was also correlated to the difference between cIVCSS and cIVCRC.
Results
cIVCRC ≥ 42% was 61.5% sensitive (95% CI, 31.58%-86.14%) and 67.1% specific (95% CI, 55.81%-77.06%) for predicting cIVCSS ≥ 42%. cIVCRC underestimated cIVCSS. The degree of discordance between cIVCRC and cIVCSS was proportional to the value of F-IVC.
Conclusions
cIVCRC and cIVCSS measures are discordant, where cIVCRC underestimates cIVCSS. The degree of discordance is directly proportional to the value of F-IVC. Therefore, we recommend that cIVCRC ≥ 42% be used to rule in, but not to rule out, fluid responsivity. Wherever possible, F-IVC should be assessed to understand the clinical relevance of cIVCRC.
Pas effet protecteur d’une checklist orale lors de l’intubation en réanimation sur les désaturations et hypotensions artérielles
https://journal.chestnet.org/article/S0012-3692(17)32685-5/fulltext
DOI: https://doi.org/10.1016/j.chest.2017.08.1163
Background
Hypoxemia and hypotension are common complications during endotracheal intubation of critically ill adults. Verbal performance of a written, preintubation checklist may prevent these complications. We compared a written, verbally performed, preintubation checklist with usual care regarding lowest arterial oxygen saturation or lowest systolic BP experienced by critically ill adults undergoing endotracheal intubation.
Methods
A multicenter trial in which 262 adults undergoing endotracheal intubation were randomized to a written, verbally performed, preintubation checklist (checklist) or no preintubation checklist (usual care). The coprimary outcomes were lowest arterial oxygen saturation and lowest systolic BP between the time of procedural medication administration and 2 min after endotracheal intubation.
Results
The median lowest arterial oxygen saturation was 92% (interquartile range [IQR], 79-98) in the checklist group vs 93% (IQR, 84-100) with usual care (P = .34). The median lowest systolic BP was 112 mm Hg (IQR, 94-133) in the checklist group vs 108 mm Hg (IQR, 90-132) in the usual care group (P = .61). There was no difference between the checklist and usual care in procedure duration (120 vs 118 s; P = .49), number of laryngoscopy attempts (one vs one attempt; P = .42), or severe life-threatening procedural complications (40.8% vs 32.6%; P = .20).
Conclusions
The verbal performance of a written, preprocedure checklist does not increase the lowest arterial oxygen saturation or lowest systolic BP during endotracheal intubation of critically ill adults compared with usual care.
Coagulopathie après une résection hépatique : incidence, cinétique et facteur de risque
Jacquenod et al., Anesthesia & Analgesia: April 2018
BACKGROUND: Hepatic surgery is a major abdominal surgery. Epidural analgesia may decrease the incidence of postoperative morbidities. Hemostatic disorders frequently occur after hepatic resection. Insertion or withdrawal (whether accidental or not) of an epidural catheter during coagulopathic state may cause an epidural hematoma. The aim of the study is to determine the incidence of coagulopathy after hepatectomy, interfering with epidural catheter removal, and to identify the risk factors related to coagulopathy.
METHODS: We performed a retrospective review of a prospective, multicenter, observational database including patients over 18 years old with a history of liver resection. Main collected data were the following: age, preexisting cirrhosis, Child-Pugh class, preoperative and postoperative coagulation profiles, extent of liver resection, blood loss, blood products transfused during surgery. International normalized ratio (INR) ≥1.5 and/or platelet count <80,000/mm3 defined coagulopathy according to the neuraxial anesthesia guidelines. A logistic regression analysis was performed to assess the association between selected factors and a coagulopathic state after hepatic resection.
RESULTS: One thousand three hundred seventy-one patients were assessed. Seven hundred fifty-nine patients had data available about postoperative coagulopathy, which was observed in 53.5% [95% confidence interval, 50.0–57.1]. Maximum derangement in INR occurred on the first postoperative day, and platelet count reached a trough peak on postoperative days 2 and 3. In the multivariable analysis, preexisting hepatic cirrhosis (odds ratio [OR] = 2.49 [1.38–4.51]; P = .003), preoperative INR ≥1.3 (OR = 2.39 [1.10–5.17]; P = .027), preoperative platelet count <150 G/L (OR = 3.03 [1.77–5.20]; P = .004), major hepatectomy (OR = 2.96 [2.07–4.23]; P < .001), and estimated intraoperative blood loss ≥1000 mL (OR = 1.85 [1.08–3.18]; P = .025) were associated with postoperative coagulopathy.
CONCLUSIONS: Coagulopathy is frequent (53.5% [95% confidence interval, 50.0–57.1]) after liver resection. Epidural analgesia seems safe in patients undergoing minor hepatic resection without preexisting hepatic cirrhosis, showing a normal preoperative INR and platelet count.
L’utilisation d’une perfusion de glucose-potassium-insuline protège de la dysfonction ventriculaire en post-opératoire de chirurgie cardiaque
doi: 10.1213/ANE.0000000000002777
BACKGROUND: Low cardiac output syndrome is a main cause of death after cardiac surgery. We sought to assess the impact of glucose–insulin–potassium (GIK) to enhance myocardial protection in moderate- to high-risk patients undergoing on-pump heart surgery.
METHODS: A randomized controlled trial was performed in adult patients (Bernstein–Parsonnet score >7) scheduled for elective aortic valve replacement and/or coronary artery bypass surgery. Patients were randomized to GIK (20 IU of insulin, 10 mEq of potassium chloride in 50 mL of glucose 40%) or saline infusion given over 60 minutes on anesthetic induction. The primary end point was postcardiotomy ventricular dysfunction (PCVD), defined as new/worsening left ventricular dysfunction requiring inotropic support (≥120 minutes). Secondary end points were the intraoperative changes in left ventricular function as assessed by transoesophageal echocardiography, postoperative troponin levels, cardiovascular and respiratory complications, and intensive care unit and hospital length of stay.
RESULTS: From 224 randomized patients, 222 were analyzed (112 and 110 in the placebo and GIK groups, respectively). GIK pretreatment was associated with a reduced occurrence of PCVD (risk ratio [RR], 0.41; 95% confidence interval [CI], 0.25–0.66). In GIK-treated patients, the left systolic ventricular function was better preserved after weaning from bypass, plasma troponin levels were lower on the first postoperative day (2.9 ng·mL−1 [interquartile range {IQR}, 1.5–6.6] vs 4.3 ng·mL−1 [IQR, 2.4–8.2]), and cardiovascular (RR, 0.69; 95% CI, 0.50–0.89) and respiratory complications (RR, 0.5; 95% CI, 0.38–0.74) were reduced, along with a shorter length of stay in intensive care unit (3 days [IQR, 2–4] vs 3.5 days [IQR, 2–7]) and in hospital (14 days [IQR, 11–18.5] vs 16 days [IQR, 12.5–23.5]), compared with placebo-treated patients.
CONCLUSIONS: GIK pretreatment was shown to attenuate PCVD and to improve clinical outcome in moderate- to high-risk patients undergoing on-pump cardiac surgery.
Bloc du Serratus après vidéo-thoracoscopie : Amélioration des scores de récupération et diminution de la consommation de morphinique
Do-Hyeong et al., Anesthesia & Analgesia: April 2018
BACKGROUND: The optimal regional technique for analgesia and improved quality of recovery after video-assisted thoracic surgery (a procedure associated with considerable postoperative pain) has not been established. The main objective in this study was to compare quality of recovery in patients undergoing serratus plane block (SPB) with either ropivacaine or normal saline on the first postoperative day. Secondary outcomes were analgesic outcomes, including postoperative pain intensity and opioid consumption.
METHODS: Ninety patients undergoing video-assisted thoracic surgery were randomized to receive ultrasound-guided SPB with 0.4 mL/kg of either 0.375% ropivacaine (SPB group) or normal saline (control group) after anesthetic induction. The primary outcome was the 40-item Quality of Recovery (QoR-40) score at 24 hours after surgery. The QoR-40 questionnaire was completed by patients the day before surgery and on postoperative days 1 and 2. Pain scores, opioid consumption, and adverse events were assessed for 2 days postoperatively.
RESULTS: Eighty-five patients completed the study: 42 in the SPB group and 43 in the control group. The global QoR-40 scores on both postoperative days 1 and 2 were significantly higher in the SPB group than in the control group (estimated mean difference 8.5, 97.5% confidence interval [CI], 2.1–15.0, and P = .003; 8.5, 97.5% CI, 2.0–15.1, and P = .004, respectively). The overall mean difference between the SPB and control groups was 8.5 (95% CI, 3.3–13.8; P = .002). Pain scores at rest and opioid consumption were significantly lower up to 6 hours after surgery in the SPB group than in the control group. Cumulative opioid consumption was significantly lower up to 24 hours postoperatively in the SPB group.
CONCLUSIONS: Single-injection SPB with ropivacaine enhanced the quality of recovery for 2 days postoperatively and improved postoperative analgesia during the early postoperative period in patients undergoing video-assisted thoracic surgery.
Méta-analyse : Esmolol comme épargneur morphinique ?
Anesthesia & Analgesia. 2018
https://insights.ovid.com/pubmed?pmid=29028742
DOI: 10.1213/ANE.0000000000002469





 6 mai 2018
6 mai 2018













 Étiquettes :
Étiquettes :