LA BIBLIO DU MOIS: Décembre 2020
LA BIBLIO DU MOIS: Décembre 2020
Pour bien commencer l’année 2021 & comme nous vous l’avions annoncé, voici le retour de la biblio du mois avec les publications immanquables de ces derniers mois !
Au menu : de l’anesthésie, de la réa, un peu de covid (mais pas trop), de l’infectiologie, et bien d’autres encore, alors régalez-vous !
LES INDÉTRÔNABLES :
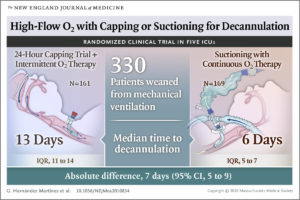
High-Flow Oxygen with Capping or Suctioning for Tracheostomy Decannulation
Référence : DOI: 10.1056/NEJMoa2010834
Quelques lignes de présentations : Quand mon patient trachéotomisé est-il prêt à être décannulé ? Sevrage avec oxygénothérapie haut débit (OHD) et bouchon sur trachéotomie ou protocole OHD et fréquence des aspirations.
Lorsque les patients avec une trachéotomie ont suffisamment évolué pour qu’une décanulation apparaisse possible il est fréquent d’obturer la trachéotomie pour une durée de 24 heures et de regarder si le patient respire par lui-même. Cette méthode pour établir si le patient est prêt à être décannulé permet-elle de meilleurs résultats qu’un protocole basé sur la fréquence des aspirations ?
Résumé article:
BACKGROUND: When patients with a tracheostomy tube reach a stage in their care at which decannulation appears to be possible, it is common practice to cap the tracheos- tomy tube for 24 hours to see whether they can breathe on their own. Whether this approach to establishing patient readiness for decannulation leads to better outcomes than one based on the frequency of airway suctioning is unclear.
METHODS In five intensive care units (ICUs), we enrolled conscious, critically ill adults who had a tracheostomy tube; patients were eligible after weaning from mechanical ventilation. In this unblinded trial, patients were randomly assigned either to un- dergo a 24-hour capping trial plus intermittent high-flow oxygen therapy (control group) or to receive continuous high-flow oxygen therapy with frequency of suc- tioning being the indicator of readiness for decannulation (intervention group). The primary outcome was the time to decannulation, compared by means of the log-rank test. Secondary outcomes included decannulation failure, weaning fail- ure, respiratory infections, sepsis, multiorgan failure, durations of stay in the ICU and hospital, and deaths in the ICU and hospital.
RESULTS The trial included 330 patients; the mean (±SD) age of the patients was 58.3±15.1 years, and 68.2% of the patients were men. A total of 161 patients were assigned to the control group and 169 to the intervention group. The time to decannulation was shorter in the intervention group than in the control group (median, 6 days [interquartile range, 5 to 7] vs. 13 days [interquartile range, 11 to 14]; absolute difference, 7 days [95% confidence interval, 5 to 9]). The incidence of pneumonia and tracheobronchitis was lower, and the duration of stay in the hospital shorter, in the intervention group than in the control group. Other secondary outcomes were similar in the two groups.
CONCLUSIONS Basing the decision to decannulate on suctioning frequency plus continuous high- flow oxygen therapy rather than on 24-hour capping trials plus intermittent high- flow oxygen therapy reduced the time to decannulation, with no evidence of a between-group difference in the incidence of decannulation failure. (REDECAP ClinicalTrials.gov number, NCT02512744.)
Percutaneous Tracheostomy
Référence : DOI: 10.1056/NEJMvcm2014884
Quelques lignes de présentations : Rappel sur les indications, contre-indications, la préparation, le positionnement et la procédure à effectuer lors de la réalisation d’une trachéotomie.
Résumé article : Vidéo descriptive
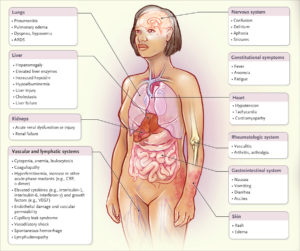
Cytokine storm
Référence : DOI: 10.1056/NEJMra2026131
Quelques lignes de présentations : Orage cytokine : état des lieux !
Qu’il soit réactionnel à un pathogène, une maladie auto-immune ou un cancer, l’orage cytokinique est responsable de situations mettant en jeu le pronostic vital. Retour sur les signes cliniques et biologiques qui le caractérise ainsi que sur les différentes cellules mises en jeu et les thérapeutiques pour y faire face.
First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial (December 12, 2020)
Référence : DOI: 10.1016/S0140-6736(20)32532-0
Quelques lignes de présentations : Étude contrôlée randomisée comparant l’intubation par laryngoscopie directe et vidéolaryngoscopie chez des enfants aux voies respiratoires normales.
Résumé :
BACKGROUND Orotracheal intubation of infants using direct laryngoscopy can be challenging. We aimed to investigate whether video laryngoscopy with a standard blade done by anaesthesia clinicians improves the first-attempt success rate of orotracheal intubation and reduces the risk of complications when compared with direct laryngoscopy.
OBJECTIVE We hypothesised that the first-attempt success rate would be higher with video laryngoscopy than with direct laryngoscopy.
DESIGN Multicentre, parallel group, randomised controlled trial. We randomly assigned patients (1:1) to video laryngoscopy or direct laryngoscopy.
POPULATION Infants without difficult airways abnormalities requiring orotracheal intubation in operating theatres at four quaternary children’s hospitals in the USA and one in Australia.
MAIN OUTCOME MEASURES The primary outcome was the proportion of infants with a successful first attempt at orotracheal intubation
RESULTS Between June 4, 2018, and Aug 19, 2019, 564 infants were randomly assigned: 282 (50%) to video laryngoscopy and 282 (50%) to direct laryngoscopy. The mean age of infants was 5·5 months (SD 3·3). 274 infants in the video laryngoscopy group and 278 infants in the direct laryngoscopy group were included in the mITT analysis. In the video laryngoscopy group, 254 (93%) infants were successfully intubated on the first attempt compared with 244 (88%) in the direct laryngoscopy group (adjusted absolute risk difference 5·5% [95% CI 0·7 to 10·3]; p=0·024). Severe complications occurred in four (2%) infants in the video laryngoscopy group compared with 15 (5%) in the direct laryngoscopy group (–3·7% [–6·5 to –0·9]; p=0·0087). Fewer oesophageal intubations occurred in the video laryngoscopy group (n=1 [<1%]) compared with in the direct laryngoscopy group (n=7 [3%]; –2·3 [–4·3 to –0·3]; p=0·028).
CONCLUSION Among anaesthetised infants, using video laryngoscopy with a standard blade improves the first-attempt success rate and reduces complications.
Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial
Référence :DOI: 10.1016/ S0140-6736(20)32466-1 / Lancet 2020; 396: 1979–93
Quelques lignes de présentations : Evaluation de l’efficacité et de la sécurité d’un vaccin (ChAdOx1 nCoV-19) contre la Covid19, notamment chez les sujets âgés.
Résumé :
BACKGROUND Older adults (aged ≥70 years) are at increased risk of severe disease and death if they develop COVID-19 and are therefore a priority for immunisation should an efficacious vaccine be developed. Immunogenicity of vaccines is often worse in older adults as a result of immunosenescence.
OBJECTIVE To assess the safety and humoral and cellular immunogenicity of a single-dose and two-dose schedule of a novel chimpanzee adenovirus-vectored vaccine, ChAdOx1 nCoV-19in adults older than 55 years.
PATIENTS Healthy adults aged 18 years and older were enrolled at two UK clinical research facilities, in an age-escalation manner, into 18–55 years, 56–69 years, and 70 years and older immunogenicity subgroups
DESIGN Single-blind, randomised, controlled, phase 2/3 trial. Within each age group, participants were randomly assigned to receive either intramuscular ChAdOx1 nCoV-19 (2·2×1010 virus particles) or a control vaccine, MenACWY, using block randomisation and stratified by age and dose group and study site.
MAIN OUTCOME MEASURES The coprimary outcomes of the trial were efficacy, as measured by the number of cases of symptomatic, virologically confirmed COVID-19, and safety, as measured by the occurrence of serious adverse events.
RESULTS Local and systemic reactions were more common in participants given ChAdOx1 nCoV-19 than in those given the control vaccine, and similar in nature to those previously reported (injection-site pain, feeling feverish, muscle ache, headache), but were less common in older adults (aged ≥56 years) than younger adults.
In participants who received two doses of vaccine, median anti-spike SARS-CoV-2 IgG responses 28 days after the boost dose were similar across the three age cohorts (standard-dose groups: 18–55 years, 20713 arbitrary units [AU]/mL [IQR 13898–33550], n=39; 56–69 years, 16170 AU/mL [10233–40353], n=26; and ≥70 years 17561 AU/mL [9705–37796], n=47; p=0·68). Neutralising antibody titres after a boost dose were similar across all age groups (median MNA80 at day 42 in the standard-dose groups: 18–55 years, 193 [IQR 113–238], n=39; 56–69 years, 144 [119–347], n=20; and ≥70 years, 161 [73–323], n=47; p=0·40). By 14 days after the boost dose, 208 (>99%) of 209 boosted participants had neutralising antibody responses. T-cell responses peaked at day 14 after a single standard dose of ChAdOx1 nCoV-19.
CONCLUSION ChAdOx1 nCoV-19 appears to be better tolerated in older adults than in younger adults and has similar immunogenicity across all age groups after a boost dose. Further assessment of the efficacy of this vaccine is warranted in all age groups and individuals with comorbidities.
Ultra-early tranexamic acid after subarachnoid haemorrhage (ULTRA): a randomised controlled trial (December 21, 2020)
Référence: DOI:https://doi.org/10.1016/S0140-6736(20)32518-6
Quelques lignes de présentation: L’acide tranexamique est jugée efficace pour la survie chez le polytraumatisé en choc hémorragique. Est ce que cette efficacité est retrouvée dans les saignements sous arachnoïdiens sur anévrysme ?
(aide à arrêter le saignement => Survie augmentée ?)
Résumé :
BACKGROUND In patients with aneurysmal subarachnoid haemorrhage, short-term antifibrinolytic therapy with tranexamic acid has been shown to reduce the risk of rebleeding. However, whether this treatment improves clinical outcome is unclear. We investigated whether ultra-early, short-term treatment with tranexamic acid improves clinical outcome at 6 months.
METHODS In this multicentre prospective, randomised, controlled, open-label trial with masked outcome assessment, adult patients with spontaneous CT-proven subarachnoid haemorrhage in eight treatment centres and 16 referring hospitals in the Netherlands were randomly assigned to treatment with tranexamic acid in addition to care as usual (tranexamic acid group) or care as usual only (control group). Tranexamic acid was started immediately after diagnosis in the presenting hospital (1 g bolus, followed by continuous infusion of 1 g every 8 h, terminated immediately before aneurysm treatment, or 24 h after start of the medication, whichever came first). The primary endpoint was clinical outcome at 6 months, assessed by the modified Rankin Scale, dichotomised into a good (0–3) or poor (4–6) clinical outcome. Both primary and safety analyses were according to intention to treat. This trial is registered at ClinicalTrials.gov, NCT02684812.
FINDINGS Between July 24, 2013, and July 29, 2019, we enrolled 955 patients; 480 patients were randomly assigned to tranexamic acid and 475 patients to the control group. In the intention-to-treat analysis, good clinical outcome was observed in 287 (60%) of 475 patients in the tranexamic acid group, and 300 (64%) of 470 patients in the control group (treatment centre adjusted odds ratio 0·86, 95% CI 0·66–1·12). Rebleeding after randomisation and before aneurysm treatment occurred in 49 (10%) patients in the tranexamic acid and in 66 (14%) patients in the control group (odds ratio 0·71, 95% CI 0·48–1·04). Other serious adverse events were comparable between groups.
CONCLUSION In patients with CT-proven subarachnoid haemorrhage, presumably caused by a ruptured aneurysm, ultra-early, short-term tranexamic acid treatment did not improve clinical outcome at 6 months, as measured by the modified Rankin Scale.
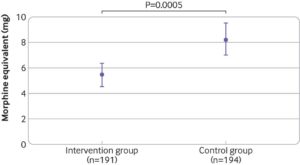
Effect of therapeutic suggestions during general anaesthesia on postoperative pain and opioid use: multicentre randomised controlled trial
Référence : Nowak et al., BMJ 2020;371:m4284 DOI: 10.1136/bmj.m4284
Quelques lignes de présentation : Hypnose sur les douleurs post-opératoires
Résumé:
OBJECTIVE To investigate the effect of therapeutic suggestions played to patients through earphones during surgery on postoperative pain and opioid use.
DESIGN Blinded randomised controlled study.
SETTING Five tertiary care hospitals in Germany.
PARTICIPANTS 385 of 400 patients consecutively recruited from January to December 2018 who were to undergo surgery for 1-3 hours under general anaesthesia. In the per protocol analysis 191 patients were included in the intervention group and 194 patients in the control group.
INTERVENTION The intervention comprised an audiotape of background music and positive suggestions based on hypnotherapeutic principles, which was played repeatedly for 20 minutes followed by 10 minutes of silence to patients through earphones during general anaesthesia. Patients in the control group were assigned to a blank tape.
MAIN OUTCOME The main outcome was dose of opioid administered by patient controlled analgesia or nurse controlled analgesia within the first postoperative 24 hours, based on regular evaluation of pain intensity on a numerical rating scale (range 0-10, with higher scores representing more severe pain).
RESULTS Compared with the control group, the intervention group required a significantly (P=0.002) lower opioid dose within 24 hours after surgery, with a median of 4.0 mg (interquartile range 0-8) morphine equivalents versus 5.3 (2-12), and an effect size (Cohen’s d) of 0.36 (95% confidence interval 0.16 to 0.56). The number of patients who needed opioids postoperatively was significantly (P=0.001) reduced in the intervention group: 121 of 191 (63%, 95% confidence interval 45% to 70%) patients in the intervention group versus 155 of 194 (80%, 74% to 85%) in the control group. The number needed to treat to avoid postoperative opioids was 6. Pain scores were consistently and significantly lower in the intervention group within 24 hours after surgery, with an average reduction of 25%. No adverse events were reported.
CONCLUSIONS Therapeutic suggestions played through earphones during general anaesthesia could provide a safe, feasible, inexpensive, and non-drug technique to reduce postoperative pain and opioid use, with the potential for more general use. Based on the finding of intraoperative perception by a considerable number of patients, surgeons and anaesthetists should be careful about background noise and conversations during surgery.
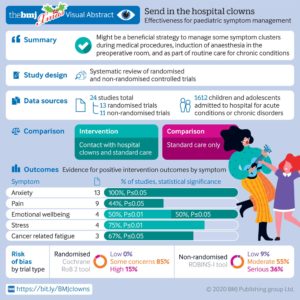
Effectiveness of hospital clowns for symptom management in paediatrics: systematic review of randomised and non-randomised controlled trials
Référence : Lopez-Junior et al., BMJ 2020;371:m4290http://dx.doi.org/10.1136/bmj.m4290
Quelques lignes de présentation : Effets des clowns en pédiatrie
Résumé:
OBJECTIVE To evaluate evidence from randomised controlled trials and non-randomised controlled trials on the effectiveness of hospital clowns for a range of symptom clusters in children and adolescents admitted to hospital with acute and chronic conditions.
DESIGN Systematic review of randomised and non-randomised controlled trials.
STUDY SELECTION Randomised and non-randomised controlled trials were peer reviewed using the following eligibility criteria: children and adolescents who were admitted to hospital for acute conditions or chronic disorders, studies comparing use of hospital clowns with standard care, and studies evaluating the effect of hospital clowns on symptom management of inpatient children and adolescents as a primary outcome.
DATA EXTRACTION AND SYNTHESIS Two investigators independently screened studies, extracted data, and appraised the risk of bias. Methodological appraisal was assessed by two investigators independently using the Jadad scale, the revised Cochrane risk-of-bias tool for randomised controlled trials (RoB 2), and the risk of bias in non-randomised studies (ROBINS-I) tool for non-randomised controlled trials.
RESULTS 24 studies (n=1612) met the inclusion criteria for data extraction and analysis. Most studies were randomised controlled trials (n=13). Anxiety was the most frequently analysed symptom (n=13), followed by pain (n=9), psychological and emotional responses and perceived wellbeing (n=4), stress (n=4), cancer related fatigue (n=3), and crying (n=2). Five studies used biomarkers, mainly cortisol, to assess stress or fatigue outcome following hospital clowns. Most of the randomised controlled trials (n=11; 85%) were rated as showing some concerns, and two trials were rated with a high risk of bias. Most non-randomised controlled trials (n=6; 55%) were rated with a moderate risk of bias according to ROBINS-I tool. Studies showed that children and adolescents who were in the presence of hospital clowns, either with or without a parent present, reported significantly less anxiety during a range of medical procedures, as well as improved psychological adjustment (P<0.05). Three studies that evaluated chronic conditions showed favourable results for the intervention of hospital clowns with significant reduction in stress, fatigue, pain, and distress (P<0.05).
CONCLUSIONS These findings suggest that the presence of hospital clowns during medical procedures, induction of anaesthesia in the preoperative room, and as part of routine care for chronic conditions might be a beneficial strategy to manage some symptom clusters. Furthermore, hospital clowns might help improve psychological wellbeing in admitted children and adolescents with acute and chronic disorders, compared with those who received only standard care.
Comparative evaluation of clinical manifestations and risk of death in patients admitted to hospital with covid-19 and seasonal influenza: cohort study
Référence : Xie et al., BMJ 2020;371:m4677http://dx.doi.org/10.1136/bmj.m4677
Quelques lignes de présentation : Comparaison Grippe vs COVID-19
Résumé :
OBJECTIVE To comparatively examine differences in risk of clinical manifestations and death among people admitted to hospital with coronavirus disease 2019 (covid-19) and seasonal influenza.
DESIGN Cohort study.
SETTING US Department of Veterans Affairs.
PARTICIPANTS Patients admitted to hospital with covid-19 between 1 February 2020 and 17 June 2020 (n=3641) and seasonal influenza between 2017 and 2019 (n=12 676).
MAIN OUTCOME Risks of clinical manifestations, healthcare resource use (including use of mechanical ventilation, admission to intensive care, and length of stay), and death, estimated using a doubly robust approach to build propensity scores that were then used along with covariates to adjust the outcome models.
RESULTS Compared with seasonal influenza, covid-19 was associated with higher risk of acute kidney injury (odds ratio 1.52, 95% confidence interval 1.37 to 1.69), incident renal replacement therapy (4.11, 3.13 to 5.40), incident insulin use (1.86, 1.62 to 2.14), severe septic shock (4.04, 3.38 to 4.83), vasopressor use (3.95, 3.46 to 4.51), pulmonary embolism (1.50, 1.18 to 1.90), deep venous thrombosis (1.50, 1.20 to 1.88), stroke (1.62, 1.17 to 2.24), acute myocarditis (7.82, 3.53 to 17.36), arrythmias and sudden cardiac death (1.76, 1.40 to 2.20), elevated troponin (1.75, 1.50 to 2.05), elevated aspartate aminotransferase (3.16, 2.91 to 3.43), elevated alanine aminotransferase (2.65, 2.43 to 2.88), and rhabdomyolysis (1.84, 1.54 to 2.18). Compared with seasonal influenza, covid-19 was also associated with higher risk of death, mechanical ventilator use, and admission to intensive care (hazard ratio 4.97, (95% confidence interval 4.42 to 5.58), 4.01 (3.53 to 4.54), and 2.41 (2.25 to 2.59), respectively) and 3.00 (2.20 to 3.80) additional days of hospital stay. Differences in rates of death per 100 patients between covid-19 and seasonal influenza were most pronounced in people over 75 years of age with chronic kidney disease or dementia and those with black race and obesity, diabetes, or chronic kidney disease.
CONCLUSIONS Among people admitted to hospital, compared with seasonal influenza, covid-19 was associated with increased risk of extrapulmonary organ dysfunction, death, and increased health resource use. The findings may inform the global discussion about the comparative risks of covid-19 and seasonal influenza and may help the ongoing effort to manage the covid-19 global pandemic.
Drug treatments for covid-19: living systematic review and network meta-analysis
Référence : https://www.bmj.com/content/370/bmj.m2980
Quelques lignes de présentation : Revue interactive traitement COVID-19
Covid-19: Doctors must be vaccinated without delay, says BMA
Référence : Abi Rimmer, BMJ 2020;371:m4964 http://dx.doi.org/10.1136/bmj.m4964
LES 100% ANESTHÉSIE :
Clinical Evaluation of a High-fidelity Upper Arm Cuff to Measure Arterial Blood Pressure during Noncardiac Surgery
Référence : doi :10.1097/ALN.0000000000003472
Présentation : La PNI surestime la PA dans les hypotensions et sous estime les hypertensions D’autres méthodes se développent pour évaluer plus précisément la PA.
Résumé :
BACKGROUND In most patients having noncardiac surgery, blood pressure is measured with the oscillometric upper arm cuff method. Although the method is noninvasive and practical, it is known to overestimate intraarterial pressure in hypotension and to underestimate it in hypertension. A high-fidelity upper arm cuff incorporating a hydraulic sensor pad was recently developed. The aim of the present study was to investigate whether noninvasive blood pressure measurements with the new high-fidelity cuff correspond to invasive measurements with a femoral artery catheter, especially at low blood pressure.
METHODS Simultaneous measurements of blood pressure recorded from a femoral arterial catheter and from the high-fidelity upper arm cuff were compared in 110 patients having major abdominal surgery or neurosurgery.
RESULTS 550 pairs of blood pressure measurements (5 pairs per patient) were considered for analysis. For mean arterial pressure measurements, the average bias was 0 mmHg, and the precision was 3 mmHg. The Pearson correlation coefficient was 0.96 (P < 0.0001; 95% CI, 0.96 to 0.97), and the percentage error was 9%. Error grid analysis showed that the proportions of mean arterial pressure measurements done with the high-fidelity cuff method were 98.4% in zone A (no risk), 1.6% in zone B (low risk) and 0% in zones C, D, and E (moderate, significant, and dangerous risk, respectively). The high-fidelity cuff method detected mean arterial pressure values less than 65 mmHg with a sensitivity of 84% (95% CI, 74 to 92%) and a specificity of 97% (95% CI, 95% to 98%). To detect changes in mean arterial pressure of more than 5 mmHg, the concordance rate between the two methods was 99.7%. Comparable accuracy and precision were observed for systolic and diastolic blood pressure measurements.
CONCLUSIONS The new high-fidelity upper arm cuff method met the current international standards in terms of accuracy and precision. It was also very accurate to track changes in blood pressure and reliably detect severe hypotension during noncardiac surgery.
Safety and 30-day outcomes of tracheostomy for COVID-19: a prospective observational cohort study
Référence : doi: 10.1016/j.bja.2020.08.023
Quelques lignes de présentations : Encore très controversée, qu’en est-il de la trachéotomie chez les patients Covid+ ? Efficace ? Dangereuse pour le patient ou le soignant ?
Résumé:
BACKGROUND The role of tracheostomy in coronavirus disease 2019 (COVID-19) is unclear, with several consensus guidelines advising against this practice.
OBJECTIVE we report outcomes in the first 100 COVID-19 patients who underwent tracheostomy at our institution.
DESIGN Prospective observational cohort study of patients confirmed to have COVID-19 who required mechanical ventilation at Queen Elizabeth Hospital, Birmingham, UK.
MAIN OUTCOME MEASURES The primary outcome measure was 30-day survival, accounting for severe organ dysfunction (Acute Physiology and Chronic Health [APACHE]-II score>17). Secondary outcomes included duration of ventilation, ICU stay, and healthcare workers directly involved in tracheostomy care acquiring COVID-19.
RESULTS A total of 164 patients with COVID-19 were admitted to the ICU between March 9, 2020 and April 21, 2020. A total of 100 patients.
Despite similar APACHE-II scores, 30-day survival was higher in 85/100 (85%) patients after tracheostomy, compared with 27/64 (42%) non-tracheostomised patients {relative risk: 3.9 (95% confidence intervals [CI]: 2.3–6.4); P<0.0001}.
In patients with APACHE-II scores ≥17, 68/100 (68%) tracheotomised patients survived, compared with 12/64 (19%) non-tracheotomised patients (P<0.001). Tracheostomy within 14 days of intubation was associated with shorter duration of ventilation (mean difference: 6.0 days [95% CI: 3.1–9.0]; P<0.0001) and ICU stay (mean difference: 6.7 days [95% CI: 3.7–9.6]; P<0.0001). No healthcare workers developed COVID-19.
CONCLUSION Independent of the severity of critical illness from COVID-19, 30-day survival was higher and ICU stay shorter in patients receiving tracheostomy. Early tracheostomy appears to be safe in COVID-19.
Comparison of vasodilatory properties between desflurane and sevoflurane using perfusion index: a randomised controlled trial
Référence : doi: 10.1016/j.bja.2020.07.050
Quelques lignes de présentations : Comparaison des propriétés vasodilatatrices du Desflurane et du Sévoflurane.
Résumé :
BACKGROUND The perfusion index (PI), calculated from the photoplethysmographic waveform, reflects peripheral vasomotor tone. As such, the PI serves as a surrogate for quantitative measures of drug-induced vasoconstriction or vasodilation.
OBJECTIVE This study aimed to compare the effect on the PI of desflurane and sevoflurane at equi-anaesthetic concentrations in patients undergoing single-agent inhalation anaesthesia, where equi-anaesthetic dose was based on the known minimum alveolar concentration of these agents.
DESIGN We randomly allocated patients scheduled for arthroscopic knee surgery to receive either desflurane or sevoflurane general anaesthesia after target-controlled induction of anaesthesia with propofol. The PI and haemodynamic data were recorded every minute for 35 min after induction of anaesthesia and after standardised nociceptive stimulation.
MAIN OUTCOME MEASURES The primary outcome was PI, compared between the groups over time (repeated-measures analysis of variance). Secondary outcomes included MAP and HR.
RESULTS Sixty-nine participants (mean [range] age: 42 yr [19–65 yr]; 49% females) were assigned to either desflurane ( n=34) or sevoflurane ( n=35). The PI remained higher under desflurane compared with sevoflurane, both before (mean difference [MD]: 3.3; 95% confidence intervals [CIs]: 2.0–4.7; P<0.001) and after tetanic stimulation (MD: 2.8; 95% CI: 2.0–3.7; P<0.001). Higher PI paralleled lower MAP in participants assigned to desflurane anaesthesia ( P<0.001), both before (MD: 8 mm Hg; 95% CI: 4–12) and after nociceptive stimulation (MD: 14 mm Hg; 95% CI: 7–22). HR was similar throughout.
CONCLUSION These findings suggest that at equipotent doses, desflurane exerts more potent vasodilatory properties and lowers blood pressure by a magnitude potentially associated with harm.
Use of etomidate in patients with heart failure undergoing noncardiac surgery
Référence : DOI: 10.1016/j.bja.2020.06.059
Quelques lignes de présentations : Est-ce dangereux d’utiliser l’étomidate chez les patients insuffisant cardiaque ? Est-ce un hypnotique particulièrement efficace du fait de ses moindres effets hémodynamiques ?
Résumé:
BACKGROUND Patients with symptomatic and asymptomatic heart failure undergoing noncardiac surgery may benefit from the haemodynamic profile of etomidate. However, the safety of etomidate in this population is unknown.
OBJECTIVE We examined anaesthesiologist variation in etomidate use and assessed its safety.
DESIGN A retrospective cohort study of 19 714 patients with heart failure undergoing noncardiac surgery at two tertiary care institutions from January 2006 to December 2017 was performed.
MAIN OUTCOME MEASURES The proportion of etomidate use among 294 anaesthesiologists was examined and adjusted risk differences (aRD) for in-hospital and 30-day mortality were calculated using physician preference for etomidate as an instrumental variable.
RESULTS Etomidate was used in 14.3% (2821/19 714) of patients. Preference for etomidate varied substantially among individual anaesthesiologists with the lowest and highest quartile users using etomidate in 0–4.7% and 20.4–66.7% of their own heart failure patients, respectively. The adjusted instrumental variable analysis showed no significant differences in the risk of in-hospital (aRD –0.2%; 95% confidence interval, –2.4%–1.9%; P=0.83) or 30 day mortality (aRD 0.2%; 95% confidence interval, –2.5%–2.9%; P=0.90).
CONCLUSION We found substantial variability in anaesthesiologists’ preference for etomidate for use in patients with heart failure undergoing noncardiac surgery. There was no association between etomidate use and in-hospital or 30-day mortality. Etomidate is not inferior to other currently used options for induction of general anaesthesia in patients with heart failure.
Epidemiology and outcome of patients admitted to intensive care after anaphylaxis in France: a retrospective multicentre study
Référence : DOI: 10.1016/j.bja.2020.08.024
Quelques lignes de présentations : Comment peut-on prédire le pronostic des patients arrivant en soins intensifs pour choc anaphylactique ?
Résumé:
BACKGROUND/OBJECTIVE Few data are available on patients who have experienced anaphylaxis and were admitted to ICUs. The purpose of this observational study was to describe the epidemiology and management of these patients.
DESIGN This was a multicentre retrospective study carried out in 23 French ICUs between 2012 and 2017. All patients who suffered anaphylaxis and were transferred to an ICU were included.
RESULTS A total of 339 patients were included, and 17 (5%) died secondary to anaphylaxis. The main triggers were drugs (77%), contrast media (11%), and food (7%). Epinephrine was administered before ICU admission in 88% of patients with Grade III anaphylaxis and 100% of patients with Grade IV anaphylaxis. Most patients with Grades III and IV anaphylaxes did not receive the recommended dose of i.v. fluid of 30 ml kg −1within the first 4 h of ICU admission. The time to epinephrine administration was not statistically different between survivors and non-survivors, but non-survivors received a higher dose of epinephrine (median: 5 [3–10] vs 3 [2–7] mg; P<0.0001), which suggests that some forms of anaphylactic shock may be resistant to epinephrine. In multivariate analysis, only lactate concentration at ICU admission was a predictor of death (odds ratio: 1.47 [1.15–1.88]; P=0.002).
CONCLUSION Lactate concentration at ICU admission appeared to be the most reliable criterion for assessing prognosis. Epinephrine is widely used during anaphylaxis, but the volume of fluid resuscitation was consistently lower than recommended.
Titre : Management practices for postdural puncture headache in obstetrics: a prospective, international, cohort study
Référence : DOI: 10.1016/j.bja.2020.07.061
Quelques lignes de présentations : Prise en charge d’une brèche méningée lors d’une péridurale: blood patch ou pas blood patch ?
Résumé:
BACKGROUND Accidental dural puncture is an uncommon complication of epidural analgesia and can cause postdural puncture headache (PDPH).
OBJECTIVE We aimed to describe management practices and outcomes after PDPH treated by epidural blood patch (EBP) or no EBP.
DESIGN Following ethics committee approval, patients who developed PDPH after accidental dural puncture were recruited from participating countries and divided into two groups, those receiving EBP or no EBP.
MAIN OUTCOME MEASURES Data registered included patient and procedure characteristics, headache symptoms and intensity, management practices, and complications. Follow-up was at 3 months.
RESULTS A total of 1001 patients from 24 countries were included, of which 647 (64.6%) received an EBP and 354 (35.4%) did not receive an EBP (no-EBP). Higher initial headache intensity was associated with greater use of EBP, odds ratio 1.29 (95% confidence interval 1.19–1.41) per pain intensity unit increase. Headache intensity declined sharply at 4h after EBP and 127 (19.3%) patients received a second EBP. On average, no or mild headache (numeric rating score≤3) was observed 7 days after diagnosis. Intracranial bleeding was diagnosed in three patients (0.46%), and backache, headache, and analgesic use were more common at 3 months in the EBP group.
CONCLUSION Management practices vary between countries, but EBP was more often used in patients with greater initial headache intensity. EBP reduced headache intensity quickly, but about 20% of patients needed a second EBP. After 7 days, most patients had no or mild headache. Backache, headache, and analgesic use were more common at 3 months in patients receiving an EBP.
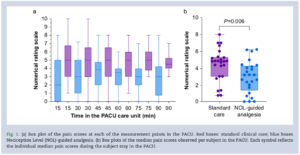
Reduced postoperative pain using Nociception Level-guided fentanyl dosing during sevoflurane anaesthesia: a randomised controlled trial
Référence : DOI: 10.1016/j.bja.2020.07.057
Résumé:
BACKGROUND The majority of postoperative patients report moderate to severe pain, possibly related to opioid underdosing or overdosing during surgery. Objective guidance of opioid dosing using the Nociception Level (NOL) index, a multiparameter artificial intelligence-driven index designed to monitor nociception during surgery, may lead to a more appropriate analgesic regimen, with effects beyond surgery.
OBJECTIVE We tested whether NOL-guided opioid dosing during general anaesthesia results in less postoperative pain.
DESIGN In this two-centre RCT, 50 patients undergoing abdominal surgery under fentanyl/sevoflurane anaesthesia were randomised to NOL-guided fentanyl dosing or standard care in which fentanyl dosing was based on haemodynamics.
MAIN OUTCOME MEASURES The primary endpoint of the study was postoperative pain assessed in the PACU.
RESULTS Median postoperative pain scores were 3.2 (inter-quartile range 1.3–4.3) and 4.8 (3.0–5.3) in NOL-guided and standard care groups, respectively (P=0.006). Postoperative morphine consumption (standard deviation) was 0.06 (0.07) mg kg−1(NOL-guided group) and 0.09 (0.09) mg kg−1 (control group; P=0.204). During surgery, fentanyl dosing was not different between groups (NOL-guided group: 6.4 [4.2] μg kg−1 vs standard care: 6.0 [2.2] μg kg−1, P=0.749), although the variation between patients was greater in the NOL-guided group (% coefficient of variation 66% in the NOL-guided group vs 37% in the standard care group).
CONCLUSION Despite absence of differences in fentanyl and morphine consumption during and after surgery,a 1.6-point improvement in postoperative pain scores was observed in the NOL-guided group.
Preoperative dexamethasone for pain relief after total knee arthroplasty: A randomised controlled trial
Référence : DOI:10.1097/EJA.0000000000001372
Quelques lignes de présentations : Dexamethasone en pré-opératoire d’une prothèse totale de genou (PTG) pour soulager les douleurs : une étude randomisée contrôlée.
Les corticostéroides peuvent réduire la douleur mais la dose optimale à administrer et le profil de sécurité restent incertains. L’objectif de cette étude est d’évaluer deux doses différentes de dexamethasone (8 mg et 16 mg) pour la gestion de la douleur post-opératoire d’une PTG ainqi que les éventuels effets secondaires associés. Etude prospective contrôlée randomisée incluant 146 malades, repartis en trois groupes : placebo, D8 et D16. Le critère de jugement principal est la douleur post-opératoire, les critères de jugements secondaires sont la consommation d’opioïdes, les paramètres physiques du genou et les effets secondaires de la dexamethasone.
Résumé :
BACKGROUND Corticosteroids can reduce pain but the optimal dose and safety profiles are still uncertain.
OBJECTIVE This study aimed to evaluate two different doses of dexamethasone for pain management and their side effects after total knee arthroplasty.
DESIGN A prospective randomised, controlled trial.
SETTING A tertiary teaching hospital in Hong Kong.
PATIENTS One hundred and forty-six patients were randomly allocated to one of three study groups.
INTERVENTIONS Before operation, patients in group D8, D16 and P received dexamethasone 8 mg, dexamethasone 16 mg and placebo (0.9% saline), respectively.
MAIN OUTCOME MEASURES The primary outcome was postoperative pain score. Secondary outcomes were opioid consumption, physical parameters of the knees and side effects of dexamethasone.
RESULTS Compared with placebo, group D16 patients had significantly less pain during maximal active flexion on post- operative day 3 [1.3 (95% CI, 2.2 to 0.31), P 1⁄4 0.005]. There was also a significant dose-dependent trend between pain scores and dexamethasone dose (P 1⁄4 0.002). Compared with placebo, patients in group D16 consumed significantly less opioid [6.4 mg (95% CI, 11.6 to 1.2), P 1⁄4 0.025] and had stronger quadriceps power on the first three postop- erative days (all P < 0.05). They also had significantly longer walking distance on postoperative day 1 [7.8 m ([95% CI, 0.85 to 14.7), P 1⁄4 0.023] with less assistance during walking on the first two postoperative days (all P < 0.029) and significantly better quality-of-recovery scores on postoperative day 1 (P1⁄40.018). There were significant dose-dependent trends between all the above parameters and dexamethasone dose (all P < 0.05). No significant differences were found in the incidence of chronic pain or knee function 3, 6 and 12 months postoperatively.
CONCLUSION Dexamethasone 16 mg given before total knee arthroplasty led to a reduction in postoperative pain, less opioid consumption, stronger quadriceps muscle power, better mobilisation and better overall quality-of-recov- ery after operation. No long-term improvement in reduction in pain and function of the knee was found.
Risk factors for ventilator-associated pneumonia due to Staphylococcus aureus in patients with severe brain injury: A multicentre retrospective cohort study
Référence : Launey et al., https://doi.org/10.1016/j.accpm.2020.01.012
https://www.sciencedirect.com/science/article/abs/pii/S235255682030271X
Quelques lignes de présentations : Facteurs protecteurs de PAVM à Staph doré
Résumé :
BACKGROUND The present study aims at identifying the risk factors for ventilator-associated pneumonia (VAP) Staphylococcus aureus (S. aureus) in patients with severe brain injury (SBI).
METHODS In this multicentre, retrospective, observational study, patients ≥ 18 year old who had SBI (Glasgow coma scale GCS score < 9) who received mechanical ventilation for at least 48 h were analysed. The main objective was to identify risk factors for S. aureus VAP vs VAP due to other pathogens and to identify risk factors for S. aureus VAP vs patients who did not experience VAP
RESULTS Eight hundred and forty-seven patients with SBI were admitted in ICU after severe traumatic brain injury (n = 489, 58%), aneurysmal SAH (n = 156, 18%), stroke (n = 27, 3%), spontaneous intracranial haemorrhage (n = 80, 9%), arteriovenous malformation rupture (n = 25, 3%), and other causes (n = 70, 8%). Three hundred fifty of 847 patients (41%) had VAP with S. aureus (n = 161) or other pathogens (n = 189). In patients with VAP, the multivariate analysis shows that age per 10 years of ageing (OR 0.80, 95% CI [0.70; 0.90]; p < 0.001) and tobacco use (OR 0.54, 95%CI [0.33;0.88]; p = 0.014) were protective factors against S. aureus. Age per 10 years of ageing remained a protective factor against S. aureus VAP vs no VAP (OR 0.80, 95%CI [0.73; 0.89], p < 0.001).
CONCLUSIONS In this retrospective study involving patients with SBI and who experienced VAP, increased age and tobacco use were protective factors against VAP due to S. aureus. Increased age remained protective against S. aureus in VAP vs no VAP analysis
Two per cent alcoholic chlorhexidine versus alcoholic five per cent povidone-iodine for the prevention of perineural catheter colonisation: The CHLOVEPI randomised, controlled trial
Référence : Harkouk et al., https://doi.org/10.1016/j.accpm.2020.100790
https://www.sciencedirect.com/science/article/abs/pii/S2352556820302769
Quelques lignes de présentations : Chlorhex 2% > Bétadine iodée sur colonisation de cathéters péri-nerveux
Résumé :
BACKGROUND Multimodal analgesia, including a regional technique using perineural catheters (PNCs), is recommended for the treatment of moderate-to-severe acute postoperative pain. Perineural catheters are at risk of bacterial colonisation. In this study, we compared the cutaneous antiseptic efficacy of 2% alcoholic chlorhexidine and povidone-iodine-alcohol for preventing the bacterial colonisation of PNCs in orthopaedic surgery.
METHODS We performed a randomised, controlled trial, comparing two cutaneous antisepsis strategies, one based on 2% alcoholic chlorhexidine and the other on povidone-iodine-5% alcohol, for placed PNCs before orthopaedic surgery. The primary endpoint was the incidence of catheter bacterial colonisation (threshold > 1000 colony-forming units/ml). The secondary endpoints were the incidence of catheter-related infections and the adverse effects of the antiseptic solutions.
RESULTS From November 2016 to May 2018, we included 113 patients in this study. The use of alcoholic chlorhexidine was associated with a lower incidence of catheter colonisation (15.5% (n = 9) versus 32.7% (n = 18); OR: 0.28 [0.09-0.77], p = 0.01). No catheter-related infections or adverse effects of antiseptic solutions were observed in either group. The risk factors associated with colonisation were a duration of catheter use ≥ 3 days (p = 0.04) and obesity (p = 0.005). The most frequently identified bacterium was Staphylococcus epidermidis.
CONCLUSION Skin disinfection with 2% alcoholic chlorhexidine decreases bacterial colonisation rates for placed perineural catheters.
Psychological Impact of COVID-19 on ICU Caregivers
Référence : Caillet et al., https://doi.org/10.1016/j.accpm.2020.08.006
https://www.sciencedirect.com/science/article/abs/pii/S2352556820302101
Quelques lignes de présentations : Impact psychologique de la COVID-19 sur les soignants en réa
Résumé :
BACKGROUND Just as every pandemic, COVID-19 could lead to emotional and psychological disturbances among caregivers, especially in the Intensive Care Unit (ICU), where significant stress related to the influx of patients, exposure to the virus and the lack of documentation on this new SARS occurred. The present study aimed at assessing the psychological impact of COVID-19 on the caregivers at the peak of the “crisis period”.
MATERIALS AND METHODS A survey using the Hospital Anxiety and Depression Scale (HADS) and Impact of Event Scale – Revised (IES-R) was proposed to the persons working in 5 ICUs of a French teaching hospital (8th of April to the 21st of April 2020). Logistic regression was performed to find independent risk factors for anxiety and post-traumatic stress disorder (PTSD). A value of p < 0.05 was considered significant.
RESULTS The incidence of anxiety and depression were 48% and 16%, respectively. PTSD symptoms were present in 27% of respondents. The independent risk factors for developing anxiety syndrome were being assigned in COVID-19 + ICU (OR = 2.081 [95% confident interval (CI), 1.035-4.184)], and not be trained in intensive care medicine, OR = 2.570 [95% CI, 1.344-4.901]. The independent risk factors for PTSD are having a history of burn-out (OR = 4.591 [95% CI, 1.464-14.397] and not being trained in ICU, (OR = 2.155 [95% CI, 1.047-4.440]).
CONCLUSION COVID-19 could have a strong impact on ICU workers. These findings should lead to prevention procedures (ICU training sessions) in persons at risk.
Unplanned admission after ambulatory anaesthesia in France: analysis of a database of 36,584 patients
Référence : Cabaton et al., https://doi.org/10.1016/j.accpm.2020.100794
Quelques lignes de présentations : Admission non prévue après une chirurgie ambulatoire
Résumé :
BACKGROUND Unplanned admission (UA) after ambulatory procedures is an unexpected event that has organisational and financial impacts. This study was undertaken to determine the current rate of UA in France and to evaluate the factors associated with the occurrence of this event.
METHODS This is a retrospective analysis of a database of 36,584 patients issued from a private hospital in France. This study received an IRB approval. All of the patients that received ambulatory anaesthesia between April 2015 and June 2017 were included in this database.
RESULTS The overall rate of UA was 1.8% (95%CI: 1.3–2.3]. Hospitalisation after endoscopic procedures (gastrointestinal endoscopy and bronchial fibroscopy) was 1.1% (95%CI: 0.3–1.9), whereas it was 2.5% (95%CI: 1.8–3.2) after surgical procedures (p < 0.01). Organisational concerns, medical reason and surgical complications accounted respectively for one third of the hospitalisations. Pain was liable in 13% of cases, whereas, PONV, residual sedation and urinary retention accounted respectively for 6.9%, 2.8% and 2.6% of cases. In a multivariate analysis, age >60 years, ASA status >2, general anaesthesia and the type of the procedures were identified risk factors.
CONCLUSIONS In this large cohort of ambulatory patients, the rate of UA remains significant. This is probably related, at least partly, to more invasive procedures scheduled in ambulatory setting. However, organisational problems occurred still frequently. Some factors appear to be easily improvable by appropriate preoperative information, better operating room scheduling and better analgesic strategy.
LES 100% RÉANIMATION :
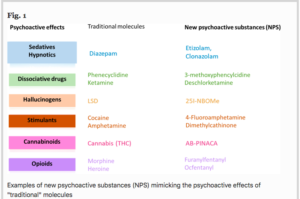
Management of pharmaceutical and recreational drug poisoning
Référence : B. Megarbane et al., https://doi.org/10.1186/s13613-020-00762-9
Quelques lignes de présentations : Recommandations 2020 de la SRLF/SFMU/STC/GFRUP sur la prise en charge des intoxications médicamenteuses et stupéfiants.
Résumé :
BACKGROUND: Poisoning is one of the leading causes of admission to the emergency department and intensive care unit. A large number of epidemiological changes have occurred over the last years such as the exponential growth of new synthetic psychoactive substances. Major progress has also been made in analytical screening and assays,
enabling the clinicians to rapidly obtain a definite diagnosis.
METHODS : A committee composed of 30 experts from five scientific societies, the Société de Réanimation de Langue Française (SRLF), the Société Française de Médecine d’Urgence (SFMU), the Société de Toxicologie Clinique (STC), the Société Française de Toxicologie Analytique (SFTA) and the Groupe Francophone de Réanimation et d’Urgences Pédiatriques
(GFRUP) evaluated eight fields: (1) severity assessment and initial triage; (2) diagnostic approach and role of toxicological analyses; (3) supportive care; (4) decontamination; (5) elimination enhancement; (6) place of antidotes; (7) specificities related to recreational drug poisoning; and (8) characteristics of cardiotoxicant poisoning. Population, Intervention,
Comparison, and Outcome (PICO) questions were reviewed and updated as needed, and evidence profiles were generated. Analysis of the literature and formulation of recommendations were then conducted according to the GRADE® methodology.
RESULTS : The SRLF-SFMU guideline panel provided 41 statements concerning the management of pharmaceutical and recreational drug poisoning. Ethanol and chemical poisoning were excluded from the scope of these recommendations.
After two rounds of discussion and various amendments, a strong consensus was reached for all recommendations. Six of these recommendations had a high level of evidence (GRADE 1±) and six had a low level of evidence (GRADE 2±). Twenty-nine recommendations were in the form of expert opinion recommendations due to the low evidences in the literature.
CONCLUSIONS : The experts reached a substantial consensus for several strong recommendations for optimal management of pharmaceutical and recreational drug poisoning, mainly regarding the conditions and effectiveness
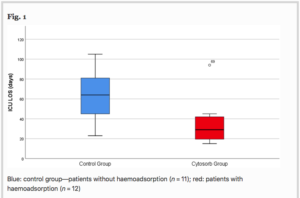
Adsorption therapy in critically ill with septic shock and acute kidney injury: a retrospective and prospective cohort study
Référence : GA. Schittek et al. , https://doi.org/10.1186/s13613-020-00772-7
Quelques lignes de présentations : Le choc septique est lié en partie à une dysrégulation immunitaire +/- cytonkinique, pouvant être responsable de nombreuses défaillances d’organes. Retirer ces cytokines pourrait aider à la guérison du choc septique, mais pas d’études encore publiées sur ce point.
Les auteurs posent ici une 1ère étude dans ce domaine, mais spécifiquenent chez les patients en choc septique avec défaillance rénale aigue.
Résumé :
BACKGROUND Haemoadsorption has been described as an effective way to control increased pro- and anti-inflammatory mediators (“cytokine storm”) in septic shock patients. No prospective or randomised clinical study has yet confirmed these results. However, no study has yet prospectively specifically investigated patients in severe septic shock with sepsis-associated acute kidney injury (SA-AKI). Therefore, we aimed to examine whether haemoadsorption could influence intensive care unit (ICU) and hospital mortality in these patients. Furthermore, we examined the influence of haemoadsorption on length of stay in the ICU and therapeutic support.
METHODS Retrospective control group and prospective intervention group design in a tertiary hospital in central Europe (Germany). Intervention was the implementation of haemoadsorption for patients in septic shock with SA-AKI. 76 patients were included in this analysis.
RESULTS Severity of illness as depicted by APACHE II was higher in patients treated with haemoadsorption. Riskadjusted ICU mortality rates (O/E ratios) did not differ significantly between the groups (0.80 vs. 0.83). We observed in patients treated with haemoadsorption a shorter LOS and shorter therapeutic support such as catecholamine dependency and duration of RRT. However, in multivariate analysis (logistic regression for mortality, competing risk for LOS), we found no significant differences between the two groups.
CONCLUSION The implementation of haemoadsorption for patients in septic shock with acute renal failure did not lead to a reduction in ICU or hospital mortality rates. Despite univariate analysis delivering some evidence for a shorter duration of ICU
Effectiveness of corticosteroids for post‑extubation stridor and extubation failure in pediatric patients: a systematic review and meta analysis
Référence : S. Kimura et al. , https://doi.org/10.1186/s13613-020-00773-6
Quelques lignes de présentations : Les corticoïdes pour le stridor post extubation et en prévention de l’échec de l’extubation sont bien prouvés efficaces chez l’adulte. Mais ces résultats ne semblent pas généralisables chez l’enfant (du fait d’une anatomie laryngée différente) => Les auteurs ont effectué une review + méta analyse des essais cliniques dans ce domaine chez les enfants
Résumé:
BACKGROUND While the results of previous meta-analyses have shown beneficial effects of corticosteroid therapy on post-extubation stridor and extubation failure in adults, these results might not be generalizable to children because of the differences in anatomy and structure. We aimed to determine the benefits of corticosteroids on those outcomes
in pediatric populations.
METHODS We searched PubMed, EMBASE, and reference lists of articles from inception until February 2019. Randomized controlled trials and observational studies on the efficacy of systemic corticosteroid administration given prior to elective extubation in mechanically ventilated pediatrics were eligible. Outcomes included post-extubation stridor
indicating laryngeal edema and extubation failures.
RESULTS A total of ten randomized controlled trials with 591 pediatric patients were included: seven of the ten studies for post-extubation stridor/suspected upper airway obstruction and nine of the ten studies for extubation failure. The estimate of pooled odds ratios (ORs) for post-extubation stridor/suspected upper airway obstruction was 0.40 (95% CI: 0.21–0.79). When analysis was restricted to trials that had explicit data for infants and explicit data for pediatric patients under 5 years old excluding infants, the estimates of pooled ORs were 0.53 (95% CI: 0.20–1.40) and 0.68 (95% CI: 0.38–1.22), respectively. For pediatric patients who received corticosteroids, there was a 0.37-fold lower odds of extubation failure than that in pediatric patients who did not receive corticosteroids (OR, 0.37; 95% CI, 0.22–0.61).
While three observational studies were included in this review, their estimates have a potential for bias and we did not perform a meta-analysis.
CONCLUSIONS Despite a relatively small sample size in each randomized controlled trial and wide ranges of ages and steroid administration regimens, our results suggest that the use of corticosteroids for prevention of post-extubation stridor and extubation failure could be considered to be acceptable in pediatric patients.
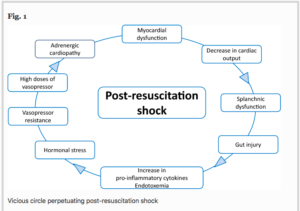
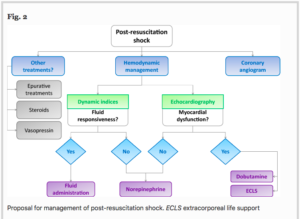
Post‑resuscitation shock: recent advances in pathophysiology and treatment
Référence M. Jozwiak et al (avec A. Cariou), https://doi.org/10.1186/s13613-020-00788-z
Quelques lignes de présentations : Petite review sur le SIRS post récupération d’arrêt cardiaque, autant sur la physiopath que sur la thérapeutique potentielle 🙂
Résumé :
A post-resuscitation shock occurs in 50–70% of patients who had a cardiac arrest. It is an early and transient complication of the post-resuscitation phase, which frequently leads to multiple-organ failure and high mortality. The pathophysiology of post-resuscitation shock is complex and results from the whole-body ischemia–reperfusion process provoked by the sequence of circulatory arrest, resuscitation manoeuvers and return of spontaneous circulation, combining a myocardial dysfunction and sepsis features, such as vasoplegia, hypovolemia and endothelial dysfunction. Similarly to septic shock, the hemodynamic management of post-resuscitation shock is based on an early and aggressive hemodynamic management, including fluid administration, vasopressors and/or inotropes.
Norepinephrine should be considered as the first-line vasopressor in order to avoid arrhythmogenic effects of other catecholamines and dobutamine is the most established inotrope in this situation. Importantly, the optimal mean arterial pressure target during the post-resuscitation shock still remains unknown and may probably vary according to patients. Mechanical circulatory support by extracorporeal membrane oxygenation can be necessary in the most severe patients, when the neurological prognosis is assumed to be favourable. Other symptomatic treatments include protective lung ventilation with a target of normoxia and normocapnia and targeted temperature management by avoiding the lowest temperature targets. Early coronary angiogram and coronary reperfusion must be considered in ST-elevation myocardial infarction (STEMI) patients with preserved neurological prognosis although the timing of coronary angiogram in non-STEMI patients is still a matter of debate. Further clinical research is needed in order to explore new therapeutic opportunities regarding inflammatory, hormonal and vascular dysfunction.
Ventilator‑associated pneumonia caused by multidrug‑resistant Gram‑negative bacteria: understanding nebulization of aminoglycosides and colistin
Référence https://doi.org/10.1007/s00134-019-05890-w
Quelques lignes de présentations : Petite review sur les antibiothérapies inhalées (par Colistine / Aminosides) pour traiter les pneumonies à bactéries multi résistantes, et savoir comment les nébuliser correctement.
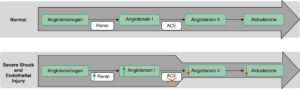
Renin and Survival in Patients Given Angiotensin II for Catecholamine-Resistant Vasodilatory Shock. A Clinical Trial
Référence : DOI: 10.1164/rccm.201911-2172OC
Quelques lignes de présentations : Intérêt de l’angiotensine II dans la prise en charge des patients choqués résistants aux cathécolamines à concentration plasmatique de rénine élevée …
Résumé:
BACKGROUND Exogenous angiotensin II increases mean arterial pressure in patients with catecholamine-resistant vasodilatory shock (CRVS). We hypothesized that renin concentrations may identify patients most likely to benefit from such therapy.
OBJECTIVE To test the kinetic changes in renin concentrations and their prognostic value in patients with CRVS.
DESIGN/OUTCOME We analyzed serum samples from patients enrolled in the ATHOS-3 (Angiotensin II for the Treatment of High-Output Shock) trial for renin, angiotensin I, and angiotensin II concentrations before the start of administration of angiotensin II or placebo and after 3 hours.
RESULTS Baseline serum renin concentration (normal range, 2.13–58.78 pg/ml) was above the upper limits of normal in 194 of 255 (76%) study patients with a median renin concentration of 172.7 pg/ml (interquartile range [IQR], 60.7 to 440.6 pg/ml), approximately threefold higher than the upper limit of normal. Renin concentrations correlated positively with angiotensin I/II ratios (r = 0.39; P < 0.001). At 3 hours after initiation of angiotensin II therapy, there was a 54.3% reduction (IQR, 37.9% to 66.5% reduction) in renin concentration compared with a 14.1% reduction (IQR, 37.6% reduction to 5.1% increase) with placebo (P < 0.0001). In patients with renin concentrations above the study population median, angiotensin II significantly reduced 28-day mortality to 28 of 55 (50.9%) patients compared with 51 of 73 patients (69.9%) treated with placebo (unstratified hazard ratio, 0.56; 95% confidence interval, 0.35 to 0.88; P = 0.012) (P = 0.048 for the interaction)
CONCLUSION The serum renin concentration is markedly elevated in CRVS and may identify patients for whom treatment with angiotensin II has a beneficial effect on clinical outcomes.
Noninvasive Ventilation Use in Critically Ill Patients with Acute Asthma Exacerbations
Référence : DOI: 10.1164/rccm.201910-2021OC
Quelques lignes de présentations : La ventilation non invasive dans l’exacerbation d’asthme, c’est oui ou c’est non?
Résumé:
BACKGROUND Noninvasive ventilation decreases the need for invasive mechanical ventilation and mortality among patients with chronic obstructive pulmonary disease but has not been well studied in asthma.
DESIGN We performed a retrospective cohort study using administrative data collected during 2010–2017 from 682 hospitals in the United States.
MAIN OUTCOME MEASURES Outcomes included receipt of invasive mechanical ventilation and in-hospital mortality.
RESULTS The study population included 53,654 participants with asthma exacerbation. During the study period, 13,540 patients received noninvasive ventilation (25.2%; 95% confidence interval [CI], 24.9–25.6%), 14,498 underwent invasive mechanical ventilation (27.0%; 95% CI, 26.7–27.4%), and 1,291 died (2.4%; 95% CI, 2.3–2.5%). Among those receiving noninvasive ventilation, 3,013 patients (22.3%; 95% CI, 21.6–23.0%) required invasive mechanical ventilation after first receiving noninvasive ventilation, 136 of whom died (4.5%; 95% CI, 3.8–5.3%). Across all models, the use of noninvasive ventilation was associated with a lower odds of receiving invasive mechanical ventilation (adjusted generalized estimating equation odds ratio, 0.36; 95% CI, 0.32–0.40) and in-hospital mortality (odds ratio, 0.48; 95% CI 0.40–0.58). Those who received noninvasive ventilation before invasive mechanical ventilation were more likely to have comorbid pneumonia and severe sepsis.
CONCLUSION Noninvasive ventilation use during asthma exacerbation was associated with improved outcomes but should be used cautiously with acute comorbid conditions.
Respiratory Tract Dysbiosis Is Associated with Worse Outcomes in Mechanically Ventilated Patients
Référence : DOI: 10.1164/rccm.201912-2441OC
Quelques lignes de présentations : Et si les déséquilibres de notre microbiote jouaient un rôle pronostic prépondérant lors des insuffisances respiratoires aiguës sous ventilation mécanique ?
Résumé :
BACKGROUND Host inflammatory responses have been strongly associated with adverse outcomes in critically ill patients, but the biologic underpinnings of such heterogeneous responses have not been defined.
OBJECTIVE We examined whether respiratory tract microbiome profiles are associated with host inflammation and clinical outcomes of acute respiratory failure.
DESIGN/OUTCOME We collected oral swabs, endotracheal aspirates (ETAs), and plasma samples from mechanically ventilated patients. We performed 16S ribosomal RNA gene sequencing to characterize upper and lower respiratory tract microbiota and classified patients into host-response subphenotypes on the basis of clinical variables and plasma biomarkers of innate immunity and inflammation. We derived diversity metrics and composition clusters with Dirichlet multinomial models and examined our data for associations with subphenotypes and clinical outcomes.
RESULTS Oral and ETA microbial communities from 301 mechanically ventilated subjects had substantial heterogeneity in α and β diversity. Dirichlet multinomial models revealed a cluster with low α diversity and enrichment for pathogens (e.g., high Staphylococcus or Pseudomonadaceae relative abundance) in 35% of ETA samples, associated with a hyperinflammatory subphenotype, worse 30-day survival, and longer time to liberation from mechanical ventilation (adjusted P < 0.05), compared with patients with higher α diversity and relative abundance of typical oral microbiota. Patients with evidence of dysbiosis (low α diversity and low relative abundance of “protective” oral-origin commensal bacteria) in both oral and ETA samples (17%, combined dysbiosis) had significantly worse 30-day survival and longer time to liberation from mechanical ventilation than patients without dysbiosis (55%; adjusted P < 0.05).
CONCLUSION Respiratory tract dysbiosis may represent an important, modifiable contributor to patient-level heterogeneity in systemic inflammatory responses and clinical outcomes.
Early Detection of Patients at Risk of Developing a Post-Traumatic Stress Disorder After an ICU Stay
Référence : doi : 10.1097/CCM.0000000000004551
Présentation : Le SSPT est défini par la présence à partir d’un mois après l’exposition à un facteur de stress (mort, menace de mort, menace réelle ou grave blessures/violences sexuelles) de symptômes d’intrusion, d’évitement, des troubles cognitifs et de l’humeur ainsi qu’une altération de la réactivité. Déterminer qui sont les patients à risque de SSPT post réanimation devient un enjeu pour bien filiariser ces patients à leur sortie du service.
Résumé:
OBJECTIVES To evaluate the diagnostic accuracy of the Impact Event Scale-Revisited assessed following ICU discharge to predict the emergence of post-traumatic stress disorder symptoms at 3 months.
DESIGN Prospective cohort study. Setting: Three medical or surgical ICU of a French university hospital (Lyon, France).
PATIENTS Patients greater than or equal to 18 years old, leaving ICU after greater than or equal to 2 nights of stay, between September 2017 and April 2018. Interventions: Patients completed the Impact Event Scale-Revisited and the Peritraumatic Dissociative Experiences Questionnaire within 8 days after ICU discharge and the Impact Event ScaleRevisited again at 3 months by phone. Patients having an Impact Event Scale-Revisited greater than or equal to 35 at 3 months were considered as having post-traumatic stress disorder symptoms.
MEASUREMENTS AND MAIN RESULTS Among the 208 patients screened, 174 were included and 145 reassessed by phone at 3 months. Among the patients included at baseline, 43% presented symptoms of acute stress. At 3 months, 13% had an Impact Event Scale-Revisited greater than or equal to 35 and 17% had a score between 12 and 34. Regarding the performance of the Impact Event Scale-Revisited performed within 8 days after the ICU discharge to predict post-traumatic stress disorder symptoms at 3 months, the area under the curve was 0.90 (95% CI, 0.80–0.99), and an Impact Event Scale-Revisited greater than or equal to 12 had a sensitivity of 90%, a specificity of 71%, a positive predictive value of 32%, and a negative predictive value of 98%. History of anxiety disorder odds ratio = 3.7 (95% CI, 1.24–11.05; p = 0.02) and Impact Event Scale-Revisited greater than or equal to 12 odds ratio = 16.57 (95% CI, 3.59–76.46; p < 0.001) were identified as risk factors for post-traumatic stress disorder symptoms.
CONCLUSIONS Impact Event Scale-Revisited assessed at ICU discharge has a good ability for the detection of patients at risk of developing post-traumatic stress disorder symptoms. Patients with history of anxiety disorder and those presenting acute stress symptoms at ICU discharge are more at risk to develop post-traumatic stress disorder symptoms. (Crit Care Med 2020; 48:1572–1579) Key Words: acute stress disorder; anxiety disorder; delirium; Impact Event Scale-Revisited; intensive care units; stress disorders, post-traumatic.
Genome-Wide Linkage Analysis of the Risk of Contracting a Bloodstream Infection in 47 Pedigrees Followed for 23 Years Assembled From a Population-Based Cohort (the HUNT Study)
Référence : Doi :10.1097/ccm.0000000000004520
Présentation : Les bactériémies sont des infections sévères et graves. La présente étude cherchait à évaluer la présence de facteur de risque génétique face à ce type d’infection.
Résumé :
OBJECTIVES Bloodstream infection is an important cause of death worldwide. The main objective of this study was to identify genetic loci linked to risk of contracting a bloodstream infection.
DESIGN Genome-wide linkage analysis. Setting: Population-based, Norwegian cohort, followed between 1995 and 2017. Subjects: Among 69,423 genotyped subjects, there were 47 families with two or more second-degree relatives with bloodstream infection in the follow-up period. There were 365 subjects in these families, of which 110 were affected. Interventions: None.
MEASUREMENTS AND MAIN RESULTS The cohort was genotyped using Illumina HumanCoreExome (Illumina, San Diego, CA) arrays. Before linkage analysis, single-nucleotide polymorphisms were pruned and clumped. In nonparametric linkage analysis using an exponential model, we found three loci with a suggestive linkage to bloodstream infection, all on chromosome 4, at 46.6 centimorgan (logarithm of odds, 2.3), 57.7 centimorgan (logarithm of odds, 3.2), and 70.0 centimorgan (logarithm of odds, 2.1). At the peak of the lead region are three genes: TLR10, TLR1, and TLR6.
CONCLUSIONS Variations in the TLR10/1/6 locus appear to be linked with the risk of contracting a bloodstream infection. (Crit Care Med 2020; 48:1580–1586) Key Words: bacteremia; genetic association studies; genetic linkage analysis; prospective studies; sepsis; toll-like receptors
The Association Between Endotracheal Tube Size and Aspiration (During Flexible Endoscopic Evaluation of Swallowing) in Acute Respiratory Failure Survivors
Référence : doi:10.1097/ccm.0000000000004554
Présentation : La taille des sondes d’intubations est-elle associée à une augmentation du risque de trouble de la déglutition post extubation.
Résumé :
OBJECTIVES To determine whether a modifiable risk factor, endotracheal tube size, is associated with the diagnosis of postextubation aspiration in survivors of acute respiratory failure.
DESIGN Prospective cohort study. Setting: ICUs at four academic tertiary care medical centers.
PATIENTS Two hundred ten patients who were at least 18 years old, admitted to an ICU, and mechanically ventilated with an endotracheal tube for longer than 48 hours were enrolled. Interventions: Within 72 hours of extubation, all patients received a flexible endoscopic evaluation of swallowing examination that entailed administration of ice, thin liquid, thick liquid, puree, and cracker boluses. Patient demographics, treatment variables, and hospital outcomes were abstracted from the patient’s medical records. Endotracheal tube size was independently selected by the patient’s treating physicians.
MEASUREMENTS AND MAIN RESULTS For each flexible endoscopic evaluation of swallowing examination, laryngeal pathology was evaluated, and for each bolus, a Penetration Aspiration Scale score was assigned. Aspiration (Penetration Aspiration Scale score ≥ 6) was further categorized into nonsilent aspiration (Penetration Aspiration Scale score = 6 or 7) and silent aspiration (Penetration Aspiration Scale score = 8). One third of patients (n = 68) aspirated (Penetration Aspiration Scale score ≥ 6) on at least one bolus, 13.6% (n = 29) exhibited silent aspiration, and 23.8% (n = 50) exhibited nonsilent aspiration. In a multivariable analysis, endotracheal tube size (≤ 7.5 vs ≥ 8.0) was significantly associated with patients exhibiting any aspiration (Penetration Aspiration Scale score ≥ 6) (p = 0.016; odds ratio = 2.17; 95% CI 1.14–4.13) and with risk of developing laryngeal granulation tissue (p = 0.02).
CONCLUSIONS Larger endotracheal tube size was associated with increased risk of aspiration and laryngeal granulation tissue. Using smaller endotracheal tubes may reduce the risk of postextubation aspiration. (Crit Care Med 2020; 48:1604–1611) Key Words: adult; airway extubation; deglutition disorders; intratracheal intubation; respiratory aspiration; respiratory distress syndrome
A Randomized Controlled Trial of Antithrombin Supplementation During Extracorporeal Membrane Oxygenation
Référence : doi : 10.1097/CCM.0000000000004590
Présentation : L’adjonction d’antithrombine exogène permet-elle de diminuer les doses d’héparine pour atteindre un niveau d’anticoagulation efficace chez les patients sous ECMO. Avec cette adjonction vois t on le risque hémorragique augmenter.
Résumé :
OBJECTIVES Supplementation of antithrombin might decrease the amount of heparin needed to achieve a given anticoagulation target during extracorporeal membrane oxygenation. However, exogenous antithrombin itself may increase the risk of bleeding. We conceived a study to evaluate the effect of antithrombin supplementation in adult patients requiring venovenous extracorporeal membrane oxygenation for respiratory failure on heparin dose, adequacy of anticoagulation, and safety.
DESIGN Prospective randomized controlled trial. Setting: ICUs of two Italian referral extracorporeal membrane oxygenation centers. Patients: Adult patients requiring venovenous extracorporeal membrane oxygenation for severe respiratory failure and unfractionated heparin for systemic anticoagulation. Interventions: Before extracorporeal membrane oxygenation start, patients were randomized to either receive antithrombin concentrate to maintain a plasmatic level 80–120% (treatment) or not (control) during the extracorporeal membrane oxygenation course.
MEASUREMENTS AND MAIN RESULTS The primary outcome was the total amount of heparin required to maintain activated partial thromboplastin time ratio 1.5–2. Secondary outcomes were anti-factor Xa, the incidence of hemorrhagic and thrombotic events, and the amount of blood products transfused. Twenty-four patients in the treatment group and 24 in the control group were included in the intention-to-treat analysis. Antithrombin was 109.5% (93.0–123.0%) in the treatment group and 84.0% (68.5–98.0%) in the control group (p = 0.001). Supplementation of antithrombin did not decrease heparin dose (13.5 international units/kg/hr [9.6–17.9 international units/kg/hr] vs 15.1 international units/kg/hr [10.7–18.3 international units/kg/hr] in the treatment and control group, respectively; p = 0.33) and anti-Factor Xa levels (0.4 international units/mL [0.3–0.5 international units/mL] vs 0.3 international units/mL [0.2–0.5 international units/mL] in the treatment group and control group respectively; p = 0.65). Bleeding, blood product transfusions, and thrombosis were not different in the two groups.
CONCLUSION Antithrombin supplementation may not decrease heparin requirement nor diminish the incidence of bleeding and/or thrombosis in adult patients on venovenous extracorporeal membrane oxygenation.
Management of Acute Ischemic Stroke
Référence : Doi : 10.1097/CCM.0000000000004597
Présentation : La prise en charge de l’AVC, un état de l’art.
Résumé:
OBJECTIVES Concise “synthetic” review of the state of the art of management of acute ischemic stroke.
DATA SOURCES Available literature on PubMed. Study Selection: We selected landmark studies, recent clinical trials, observational studies, and professional guidelines on the management of stroke including the last 10 years.
DATA EXTRACTION Eligible studies were identified and results leading to guideline recommendations were summarized.
DATA SYNTHESIS Stroke mortality has been declining over the past 6 decades, and as a result, stroke has fallen from the second to the fifth leading cause of death in the United States. This trend may follow recent advances in the management of stroke, which highlight the importance of early recognition and early revascularization. Recent studies have shown that early recognition, emergency interventional treatment of acute ischemic stroke, and treatment in dedicated stroke centers can significantly reduce stroke-related morbidity and mortality. However, stroke remains the second leading cause of death worldwide and the number one cause for acquired long-term disability, resulting in a global annual economic burden.
CONCLUSIONS Appropriate treatment of ischemic stroke is essential in the reduction of mortality and morbidity. Management of stroke involves a multidisciplinary approach that starts and extends beyond hospital admission.
Improved Oxygenation After Prone Positioning May Be a Predictor of Survival in Patients With Acute Respiratory Distress Syndrome
Référence : doi: 10.1097/CCM.0000000000004611
Présentation : Le P/F du premier DV un indice de mortalité de mortalité pertinent dans le SDRA.
Résumé :
OBJECTIVES Prone position ventilation improves oxygenation and reduces the mortality of patients with severe acute respiratory distress syndrome. However, there is limited evidence about which patients would gain most survival benefit from prone positioning. Herein, we investigated whether the improvement in oxygenation after prone positioning is associated with survival and aimed to identify patients who will gain most survival benefit from prone positioning in patients with acute respiratory distress syndrome.
DESIGN A retrospective cohort study.Setting: Medical ICU at a tertiary academic hospital between 2014 and 2020.
PATIENTS Adult patients receiving prone positioning for moderate-to-severe acute respiratory distress syndrome.Interventions: None.
MEASUREMENTS AND MAIN RESULTS The main outcomes were ICU and 28-day mortality. A total of 116 patients receiving prone positioning were included, of whom 45 (38.8%) were ICU survivors. Although there was no difference in Pao2:Fio2 ratio before the first prone session between ICU survivors and nonsurvivors, ICU survivors had a higher Pao2:Fio2 ratio after prone positioning than nonsurvivors, with significant between-group difference (p < 0.001). The area under the receiver operating characteristic curve of the percentage change in the Pao2:Fio2 ratio between the baseline and 8–12 hours after the first prone positioning to predict ICU mortality was 0.87 (95% CI, 0.80–0.94), with an optimal cutoff value of 53.5% (sensitivity, 91.5%; specificity, 73.3%). Prone responders were defined as an increase in Pao2:Fio2 ratio of greater than or equal to 53.5%. In the multivariate Cox regression analysis, prone responders (hazard ratio, 0.11; 95% CI, 0.05–0.25), immunocompromised condition (hazard ratio, 2.15; 95% CI, 1.15–4.03), and Sequential Organ Failure Assessment score (hazard ratio, 1.16; 95% CI, 1.06–1.27) were significantly associated with 28-day mortality.
CONCLUSIONS The Pao2 : Fio2 ratio after the first prone positioning differed significantly between ICU survivors and nonsurvivors. The improvement in oxygenation after the first prone positioning was a significant predictor of survival in patients with moderate-to-severe acute respiratory distress syndrome.
Evaluating the Cost-Effectiveness of the ABCDE Bundle: Impact of Bundle Adherence on Inpatient and 1-Year Mortality and Costs of Care
Référence : Doi :10.1097/ccm.0000000000004609
Présentation : L’Impact d’un ensemble de mesures sur la mortalité intra hospitalière et à 1 an.
Résumé :
OBJECTIVES Growing evidence supports the Awakening and Breathing Coordination, Delirium monitoring/management, and Early exercise/mobility (ABCDE) bundle processes as improving a number of short- and long-term clinical outcomes for patients requiring ICU care. To assess the cost-effectiveness of this intervention, we determined the impact of ABCDE bundle adherence on inpatient and 1-year mortality, quality-adjusted life-years, length of stay, and costs of care. Design: We conducted a 2-year, prospective, cost-effectiveness study in 12 adult ICUs in six hospitals belonging to a large, integrated healthcare delivery system.
SETTING Hospitals included a large, urban tertiary referral center and five community hospitals. ICUs included medical/surgical, trauma, neurologic, and cardiac care units.
PATIENTS: The study included 2,953 patients, 18 years old or older, with an ICU stay greater than 24 hours, who were on a ventilator for more than 24 hours and less than 14 days. INTERVENTION ABCDE bundle. Measurements and Main Results: We used propensity scoreadjusted regression models to determine the impact of high bundle adherence on inpatient mortality, discharge status, length of stay, and costs. A Markov model was used to estimate the potential effect of improved bundle adherence on healthcare costs and quality-adjusted life-years in the year following ICU admission.
RESULTS We found that patients with high ABCDE bundle adherence (≥ 60%) had significantly decreased odds of inpatient mortality (odds ratio 0.28) and significantly higher costs ($3,920) of inpatient care. The incremental cost-effectiveness ratio of high bundle adherence was $15,077 (95% CI, $13,675–$16,479) per life saved and $1,057 per life-year saved. High bundle adherence was associated with a 0.12 increase in quality-adjusted life-years, a $4,949 increase in 1-year care costs, and an incremental cost-effectiveness ratio of $42,120 per quality-adjusted life-year.
CONCLUSIONS The ABCDE bundle appears to be a cost-effective means to reduce in-hospital and 1-year mortality for patients with an ICU stay.
DU CÔTÉ DES AUTRES SPÉCIALITÉS :
PROPHETIC: Prospective Identification of Pneumonia in Hospitalized Patients in the Intensive Care Unit
Référence : Stephen P. Bergin. et al DOI : https://doi.org/10.1016/j.chest.2020.06.034
Présentation : Il s’agit d’une étude exposant la difficulté de réaliser un diagnostic courant en réanimation : celui de la VAP ou HAP. Les auteurs se posent la question d’identifier les patients à haut risque de développer ce type d’infection. Certes, ce ne sont pas les premiers à avoir recherché les facteurs de risque de VAP et la littérature sur le sujet est abondante. Seulement 37 % des patients traités rencontraient les critères actuels de VAP ou HAP. Problème de définition ? de pratique ?
Résumé :
BACKGROUND Pneumonia is the leading infection-related cause of death. Using simple clinical criteria and contemporary epidemiology to identify patients at high risk of nosocomial pneumonia should enhance prevention efforts and facilitate development of new treatments in clinical trials.
RESEARCH QUESTION What are the clinical criteria and contemporary epidemiology trends helpful in identifying patients at high risk of nosocomial pneumonia?
STUDY DESIGNS AND METHODS Within the intensive care units of 28 United States hospitals, we conducted a prospective cohort study among adults hospitalized more than 48 hours and considered high risk for pneumonia (defined as treatment with invasive or noninvasive ventilatory support or high levels of supplemental oxygen). We estimated the proportion of high- risk patients developing nosocomial pneumonia. Using multivariable logistic regression, we identified patient characteristics and treatment exposures associated with increased risk of pneumonia development during the intensive care unit admission.
RESULTS Between February 6, 2016 and October 7, 2016, 4613 high-risk patients were enrolled. Among 1464/4613 (32%) high-risk patients treated for possible nosocomial pneumonia, 537/1464 (37%) met the study pneumonia definition. Among high-risk patients, a multivariable logistic model was developed to identify key patient characteristics and treatment exposures associated with increased risk of nosocomial pneumonia development (c-statistic 0.709, 95% confidence interval 0.686 to 0.731). Key factors associated with increased odds of nosocomial pneumonia included an admission diagnosis of trauma or cerebrovascular accident, receipt of enteral nutrition, documented aspiration risk, and receipt of systemic antibacterials within the preceding 90 days.
INTERPRETATION Treatment for nosocomial pneumonia is common among intensive care unit patients receiving high levels of respiratory support, yet more than half of patients treated do not fulfill standard diagnostic criteria for pneumonia. Application of simple clinical criteria may improve the feasibility of clinical trials of pneumonia prevention and treatment by facilitating prospective identification of patients at highest risk.
Early Changes Over Time in the Radiographic Assessment of Lung Edema Score Are Associated With Survival in ARDS
Référence : Matthieu Jabaudon et al., https://doi.org/10.1016/j.chest.2020.06.070 (open access)
Présentation : Outil simple, disponible au lit du malade : la radio de thorax comme marqueur pronostic à l’heure des techniques ultrasoniques. L’évolution de la gravité de l’atteinte radiologique dans l’ARDS, de J1 à J3, est indépendamment associée à la mortalité.
Résumé :
BACKGROUND The Radiographic Assessment of Lung Edema (RALE) score is associated with the severity of ARDS, and treatments targeted at reducing pulmonary edema such as conservative fluid management cause a reduction in RALE score over time.
RESEARCH QUESTION Are early changes in RALE score over time associated with survival in patients with ARDS?
STUDY DESIGN AND METHODS Data from patients enrolled in three centers in the Lung Imaging for Ventilation sEtting in ARDS (LIVE) trial with available chest radiographs at baseline (day 0) and days 2 or 3 were used. The RALE was scored by two independent reviewers. The primary end point was death by day 90, considering RALE score both at baseline and as a time-varying covariate in a marginal Cox survival model.
RESULTS RALE was scored from 135, 64, and 88 radiographs on days 0, 2, and 3, respectively. Both baseline RALE (hazard ratio [HR] for each one-point increment, 1.04; 95% CI, 1.01-1.08; P = .006) and the change in RALE over time (HR for each one-point decrease per unit of time, 0.99; 95% CI, 0.99-0.99; P = .03) were associated with death by day 90, even after adjustment for age, sex, BMI, Simplified Acute Physiology Score II, vasopressor use, and total volume of fluids received since study entry.
INTERPRETATION The change in RALE during the first days after ARDS onset is independently associated with survival and may be useful as a surrogate end point in future clinical trials of new therapeutics in ARDS.
Dose addition of intravenous metronidazole to oral vancomycin improve outcomes in Clostridioides difficile infection?
Référence : Wang. et al. DOI : https://doi.org/10.1093/cid/ciz1115
Présentation : En France, les recommandations pour le traitement d’une diarrhée à C. difficiles est la vancomycine PO seule, alors qu’avant on utilisait le métronidazole. Est-ce que l’association des 2 couvrirait certaines résistances ?
Résumé :
BACKGROUND Guidelines recommend adding intravenous (IV) metronidazole to oral vancomycin for fulminant Clostridioides difficile infection (CDI). In this study, we compared dual therapy with IV metronidazole and vancomycin vs vancomycin monotherapy. We assessed prevalence of use and effectiveness of dual therapy in nonfulminant and fulminant CDI.
METHODS This was a 2-center retrospective study conducted from 2010 to 2018. Adult inpatients were included if they had a positive C. difficile polymerase chain reaction (PCR) performed on an unformed stool and received vancomycin within 2 days of testing. Patients were classified as having received dual therapy if IV metronidazole was given within the same time window, and otherwise classified as vancomycin monotherapy. The primary outcome was death or colectomy within 90 days after the index test. Logistic regression modeling was used to adjust for CDI severity and other established predictors of CDI outcomes. CDI recurrence was examined as a secondary outcome, adjusting for death as a competing risk.
RESULTS The study included 2114 patients (dual therapy, 993; monotherapy, 1121); 23% met the primary outcome. There was no association between dual therapy and the primary outcome (adjusted odds ratio [aOR], 1.07; 95% confidence interval [CI], .79–1.45), which remained true when the analysis was restricted to patients with fulminant CDI (aOR, 1.17; 95% CI, .65–2.10). There was also no association between dual therapy and CDI recurrence.
CONCLUSIONS Dual therapy with IV metronidazole and vancomycin was common for nonfulminant and fulminant CDI but was not associated with improved outcomes compared with vancomycin alone.
Acute Cerebrovascular Events With COVID-19 Infection
Référence : Dhaamon et al., https://doi.org/10.1161/STROKEAHA.120.031668 Stroke. 2021;52:48–56,
https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.031668
Présentation : AVC chez patients atteints de COVID-19
Résumé :
BACKGROUND AND PURPOSE Coronavirus disease 2019 (COVID-19) has been associated with an increased incidence of thrombotic events, including stroke. However, characteristics and outcomes of COVID-19 patients with stroke are not well known.
METHODS We conducted a retrospective observational study of risk factors, stroke characteristics, and short-term outcomes in a large health system in New York City. We included consecutively admitted patients with acute cerebrovascular events from March 1, 2020 through April 30, 2020. Data were stratified by COVID-19 status, and demographic variables, medical comorbidities, stroke characteristics, imaging results, and in-hospital outcomes were examined. Among COVID-19-positive patients, we also summarized laboratory test results.
RESULTS Of 277 patients with stroke, 105 (38.0%) were COVID-19-positive. Compared with COVID-19-negative patients, COVID-19-positive patients were more likely to have a cryptogenic (51.8% versus 22.3%, P<0.0001) stroke cause and were more likely to suffer ischemic stroke in the temporal (P=0.02), parietal (P=0.002), occipital (P=0.002), and cerebellar (P=0.028) regions. In COVID-19-positive patients, mean coagulation markers were slightly elevated (prothrombin time 15.4±3.6 seconds, partial thromboplastin time 38.6±24.5 seconds, and international normalized ratio 1.4±1.3). Outcomes were worse among COVID-19-positive patients, including longer length of stay (P<0.0001), greater percentage requiring intensive care unit care (P=0.017), and greater rate of neurological worsening during admission (P<0.0001); additionally, more COVID-19-positive patients suffered in-hospital death (33% versus 12.9%, P<0.0001).
CONCLUSIONS Baseline characteristics in patients with stroke were similar comparing those with and without COVID-19. However, COVID-19-positive patients were more likely to experience stroke in a lobar location, more commonly had a cryptogenic cause, and had worse outcomes.
Avec articles associés :
- Thrombectomie sur ces AVC post-COVID : https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.031514
- Tri : https://www.ahajournals.org/doi/10.1161/STROKEAHA.120.031467





 9 janvier 2021
9 janvier 2021