LA BIBLIO DE L’AJAR: Nov/Dec 2021
L’AJAR Paris continue de vous gâter pour les fêtes avec ce petit cadeau tombé du traineau: la fameuse Biblio!
On vous a sélectionné le grand cru de ces dernières semaines, avec peut-être la réponse aux questions qui vous turlupinent depuis toujours: l’ALR fait-elle mieux que l’AG pour la chir de hanche en terme de delirium postop? Quid de la tropoHS dans la Chir non-cardiaque chez le patient à risque? De la sédation inhalée en réa? De l’effet neuro protecteur du Dexdor? Avec comme cerise sur la bûche des reviews comme on les aimes sur l’HTAP, les conséquences d’une hypoTA par organe, du monitorage hémodynamique en chir non-cardiaque.. Et même de nouvelles reco pour le jeûne pré-op de l’enfant.

Les indétrônables
✦ Spinal Anesthesia or General Anesthesia for Hip Surgery in Older Adults
DOI: 10.1056/NEJMoa2113514
Rachi vs AG dans la chirurgie de hanche chez le sujet âgé: NS sur la survie et la déambulation à 2mois, le délirium postop..
BACKGROUND
The effects of spinal anesthesia as compared with general anesthesia on the ability to walk in older adults undergoing surgery for hip fracture have not been well studied.
METHODS
We conducted a pragmatic, randomized superiority trial to evaluate spinal anesthesia as compared with general anesthesia in previously ambulatory patients 50 years of age or older who were undergoing surgery for hip fracture at 46 U.S. and Canadian hospitals. Patients were randomly assigned in a 1:1 ratio to receive spinal or general anesthesia. The primary outcome was a composite of death or an inability to walk approximately 10 ft (3 m) independently or with a walker or cane at 60 days after randomization. Secondary outcomes included death within 60 days, delirium, time to discharge, and ambulation at 60 days.
RESULTS
A total of 1600 patients were enrolled; 795 were assigned to receive spinal anesthesia and 805 to receive general anesthesia. The mean age was 78 years, and 67.0% of the patients were women. A total of 666 patients (83.8%) assigned to spinal anesthesia and 769 patients (95.5%) assigned to general anesthesia received their assigned anesthesia. Among patients in the modified intention-to-treat population for whom data were available, the composite primary outcome occurred in 132 of 712 patients (18.5%) in the spinal anesthesia group and 132 of 733 (18.0%) in the general anesthesia group (relative risk, 1.03; 95% confidence interval [CI], 0.84 to 1.27; P=0.83). An inability to walk independently at 60 days was reported in 104 of 684 patients (15.2%) and 101 of 702 patients (14.4%), respectively (relative risk, 1.06; 95% CI, 0.82 to 1.36), and death within 60 days occurred in 30 of 768 (3.9%) and 32 of 784 (4.1%), respectively (relative risk, 0.97; 95% CI, 0.59 to 1.57). Delirium occurred in 130 of 633 patients (20.5%) in the spinal anesthesia group and in 124 of 629 (19.7%) in the general anesthesia group (relative risk, 1.04; 95% CI, 0.84 to 1.30).
CONCLUSIONS
Spinal anesthesia for hip-fracture surgery in older adults was not superior to general anesthesia with respect to survival and recovery of ambulation at 60 days. The incidence of postoperative delirium was similar with the two types of anesthesia.
✦ Insights into Salt Handling and Blood Pressure: Review
DOI: 10.1056/NEJMra2030212
Une petite review qui revient à la base de la relation sel / PA, ça ne fait jamais de mal!
Salt intake is associated with blood pressure, but the relationship is complex. This review highlights the interplay among renal salt transport, salt storage in the skin and interstitium, vascular adaptation to changes in the salt concentration, and neurohormonal signaling.
✦ Milvexian for the Prevention of Venous Thromboembolism
DOI: 10.1056/NEJMoa2113194
Un nouvel anticoagulant oral à l’étude en préventif de MTEV à l’issue d’une arthroplastie de genou: le Milvexian un anti-XIa vs Lovenox. Résultats encourageants pour une phase 2!
BACKGROUND
Factor XIa inhibitors for the prevention and treatment of venous and arterial thromboembolism may be more effective and result in less bleeding than conventional anticoagulants. Additional data are needed regarding the efficacy and safety of milvexian, an oral factor XIa inhibitor.
METHODS
In this parallel-group, phase 2 trial, we randomly assigned 1242 patients undergoing knee arthroplasty to receive one of seven postoperative regimens of milvexian (25 mg, 50 mg, 100 mg, or 200 mg twice daily or 25 mg, 50 mg, or 200 mg once daily) or enoxaparin (40 mg once daily). The primary efficacy outcome was venous thromboembolism (which was a composite of asymptomatic deep-vein thrombosis, confirmed symptomatic venous thromboembolism, or death from any cause). The principal safety outcome was bleeding.
RESULTS
Among the patients receiving milvexian twice daily, venous thromboembolism developed in 27 of 129 (21%) taking 25 mg, in 14 of 124 (11%) taking 50 mg, in 12 of 134 (9%) taking 100 mg, and in 10 of 131 (8%) taking 200 mg. Among those receiving milvexian once daily, venous thromboembolism developed in 7 of 28 (25%) taking 25 mg, in 30 of 127 (24%) taking 50 mg, and in 8 of 123 (7%) taking 200 mg, as compared with 54 of 252 patients (21%) taking enoxaparin. The dose–response relationship with twice-daily milvexian was significant (one-sided P<0.001), and the 12% incidence of venous thromboembolism with twice-daily milvexian was significantly lower than the prespecified benchmark of 30% (one-sided P<0.001). Bleeding of any severity occurred in 38 of 923 patients (4%) taking milvexian and in 12 of 296 patients (4%) taking enoxaparin; major or clinically relevant nonmajor bleeding occurred in 1% and 2%, respectively; and serious adverse events were reported in 2% and 4%, respectively.
CONCLUSIONS
Postoperative factor XIa inhibition with oral milvexian in patients undergoing knee arthroplasty was effective for the prevention of venous thromboembolism and was associated with a low risk of bleeding.
✦ Pulmonary Arterial Hypertension: Review
DOI: 10.1056/NEJMra2000348
Une review spéciale HTAP: ce qu’on sait en cette fin 2021.
Without effective treatment, pulmonary arterial hypertension results in high morbidity and mortality. This review discusses the pathogenesis of the disorder, the thorough clinical evaluation required to establish the diagnosis, available therapies, and future directions.
✦ Postoperative continuous positive airway pressure to prevent pneumonia, re-intubation, and death after major abdominal surgery (PRISM): a multicentre, open-label, randomised, phase 3 trial
DOI: 10.1016/S2213-2600(21)00089-8
CPAP en post-opératoire des chirurgies abdominales, pour diminuer les complications respiratoires (pneumonie, réintubation, décès). Pas suffisamment de preuve pour la recommander en prophylactique.
Background: Respiratory complications are an important cause of postoperative morbidity. We aimed to investigate whether continuous positive airway pressure (CPAP) administered immediately after major abdominal surgery could prevent postoperative morbidity.
Methods: PRISM was an open-label, randomised, phase 3 trial done at 70 hospitals across six countries. Patients aged 50 years or older who were undergoing elective major open abdominal surgery were randomly assigned (1:1) to receive CPAP within 4 h of the end of surgery or usual postoperative care. Patients were randomly assigned using a computer-generated minimisation algorithm with inbuilt concealment. The primary outcome was a composite of pneumonia, endotracheal re-intubation, or death within 30 days after randomisation, assessed in the intention-to-treat population. Safety was assessed in all patients who received CPAP. The trial is registered with the ISRCTN registry, ISRCTN56012545.
Findings: Between Feb 8, 2016, and Nov 11, 2019, 4806 patients were randomly assigned (2405 to the CPAP group and 2401 to the usual care group), of whom 4793 were included in the primary analysis (2396 in the CPAP group and 2397 in the usual care group). 195 (8·1%) of 2396 patients in the CPAP group and 197 (8·2%) of 2397 patients in the usual care group met the composite primary outcome (adjusted odds ratio 1·01 [95% CI 0·81-1·24]; p=0·95). 200 (8·9%) of 2241 patients in the CPAP group had adverse events. The most common adverse events were claustrophobia (78 [3·5%] of 2241 patients), oronasal dryness (43 [1·9%]), excessive air leak (36 [1·6%]), vomiting (26 [1·2%]), and pain (24 [1·1%]). There were two serious adverse events: one patient had significant hearing loss and one patient had obstruction of their venous catheter caused by a CPAP hood, which resulted in transient haemodynamic instability. Interpretation: In this large clinical effectiveness trial, CPAP did not reduce the incidence of pneumonia, endotracheal re-intubation, or death after major abdominal surgery. Although CPAP has an important role in the treatment of respiratory failure after surgery, routine use of prophylactic post-operative CPAP is not recommended.
✦ Inhaled isoflurane via the anaesthetic conserving device versus propofol for sedation of invasively ventilated patients in intensive care units in Germany and Slovenia: an open-label, phase 3, randomised controlled, non-inferiority trial
DOI: 10.1016/S2213-2600(21)00323-4
Comparaison de l’isoflurane au propofol pour la sédation des patients en réanimation. Non seulement l’isoflurane n’a pas l’air de faire moins bien, mais il semblerait en plus qu’il présente quelques avantages …
Background
Previous studies indicate that isoflurane could be useful for the sedation of patients in the intensive care unit (ICU), but prospective studies evaluating isoflurane’s efficacy have been small. The aim of this study was to test whether the sedation with isoflurane was non-inferior to sedation with propofol.
Methods
This phase 3, randomised, controlled, open-label non-inferiority trial evaluated the efficacy and safety of up to 54 h of isoflurane compared with propofol in adults (aged ≥18 years) who were invasively ventilated in ICUs in Germany (21 sites) and Slovenia (three sites). Patients were randomly assigned (1:1) to isoflurane inhalation via the Sedaconda anaesthetic conserving device (ACD; Sedana Medical AB, Danderyd, Sweden; ACD-L [dead space 100 mL] or ACD-S [dead space 50 mL]) or intravenous propofol infusion (20 mg/mL) for 48 h (range 42-54) using permuted block randomisation with a centralised electronic randomisation system. The primary endpoint was percentage of time in Richmond Agitation-Sedation Scale (RASS) range -1 to -4, assessed in eligible participants with at least 12 h sedation (the per-protocol population), five or more RASS measurements, and no major protocol violations, with a non-inferiority margin of 15%. Key secondary endpoints were opioid requirements, spontaneous breathing, time to wake-up and extubation, and adverse events. Safety was assessed in all patients who received at least one dose. The trial is complete and registered with EudraCT, 2016-004551-67.
Findings
Between July 2, 2017, and Jan 12, 2020, 338 patients were enrolled and 301 (89%) were randomly assigned to isoflurane (n=150) or propofol (n=151). 146 patients (97%) in each group completed the 24-h follow-up. 146 (97%) patients in the isoflurane group and 148 (98%) of patients in the propofol group were included in the per-protocol analysis of the primary endpoint. Least-squares mean percentage of time in RASS target range was 90·7% (95% CI 86·8-94·6) for isoflurane and 91·1% (87·2-95·1) for propofol. With isoflurane sedation, opioid dose intensity was 29% lower than with propofol for the overall sedation period (0·22 [0·12-0·34] vs 0·32 [0·21-0·42] mg/kg per h morphine equivalent dose, p=0·0036) and spontaneous breathing was more frequent on day 1 (odds ratio [OR] 1·72 [1·12-2·64], generalised mixed linear model p=0·013, with estimated rates of 50% of observations with isoflurane vs 37% with propofol). Extubation times were short and median wake-up was significantly faster after isoflurane on day 2 (20 min [IQR 10-30] vs 30 min [11-120]; Cox regression p=0·0011). The most common adverse events by treatment group (isoflurane vs propofol) were: hypertension (ten [7%] of 150 vs two [1%] of 151), delirium (eight [5%] vs seven [5%]), oliguria (seven [5%] vs six [4%]), and atrial fibrillation (five [3%] vs four [3%]).
Interpretation
These results support the use of isoflurane in invasively ventilated patients who have a clinical need for sedation.
✦ Effect of Regional vs General Anesthesia on Incidence of Postoperative Delirium in Older Patients Undergoing Hip Fracture Surgery
The RAGA Randomized Trial
L’ALR dans la chir de hanche du sujet âgé: fait-elle mieux que l’AG dans la survenue de délirium postop? Pas dans cette étude chinoise qui évalue le délirium par le CAM du moins.
Importance In adults undergoing hip fracture surgery, regional anesthesia may reduce postoperative delirium, but there is uncertainty about its effectiveness.
Objective To investigate, in older adults undergoing surgical repair for hip fracture, the effects of regional anesthesia on the incidence of postoperative delirium compared with general anesthesia.
Design, Setting, and Participants A randomized, allocation-concealed, open-label, multicenter clinical trial of 950 patients, aged 65 years and older, with or without preexisting dementia, and a fragility hip fracture requiring surgical repair from 9 university teaching hospitals in Southeastern China. Participants were enrolled between October 2014 and September 2018; 30-day follow-up ended November 2018.
Interventions Patients were randomized to receive either regional anesthesia (spinal, epidural, or both techniques combined with no sedation; n = 476) or general anesthesia (intravenous, inhalational, or combined anesthetic agents; n = 474).
Main Outcomes and Measures Primary outcome was incidence of delirium during the first 7 postoperative days. Secondary outcomes analyzed in this article include delirium severity, duration, and subtype; postoperative pain score; length of hospitalization; 30-day all-cause mortality; and complications.
Results Among 950 randomized patients (mean age, 76.5 years; 247 [26.8%] male), 941 were evaluable for the primary outcome (6 canceled surgery and 3 withdrew consent). Postoperative delirium occurred in 29 (6.2%) in the regional anesthesia group vs 24 (5.1%) in the general anesthesia group (unadjusted risk difference [RD], 1.1%; 95% CI, –1.7% to 3.8%; P = .48; unadjusted relative risk [RR], 1.2 [95% CI, 0.7 to 2.0]; P = .57]). Mean severity score of delirium was 23.0 vs 24.1, respectively (unadjusted difference, –1.1; 95% CI, –4.6 to 3.1). A single delirium episode occurred in 16 (3.4%) vs 10 (2.1%) (unadjusted RD, 1.1%; 95% CI, –1.7% to 3.9%; RR, 1.6 [95% CI, 0.7 to 3.5]). Hypoactive subtype in 11 (37.9%) vs 5 (20.8%) (RD, 11.5; 95% CI, –11.0% to 35.7%; RR, 2.2 [95% CI, 0.8 to 6.3]). Median worst pain score was 0 (IQR, 0 to 20) vs 0 (IQR, 0 to 10) (difference 0; 95% CI, 0 to 0). Median length of hospitalization was 7 days (IQR, 5 to 10) vs 7 days (IQR, 6 to 10) (difference 0; 95% CI, 0 to 0). Death occurred in 8 (1.7%) vs 4 (0.9%) (unadjusted RD, –0.8%; 95% CI, –2.2% to 0.7%; RR, 2.0 [95% CI, 0.6 to 6.5]). Adverse events were reported in 106 episodes in the regional anesthesia group and 102 in the general anesthesia group; the most frequently reported adverse events were nausea and vomiting (47 [44.3%] vs 34 [33.3%]) and postoperative hypotension (13 [12.3%] vs 10 [9.8%]).
Conclusions and Relevance In patients aged 65 years and older undergoing hip fracture surgery, regional anesthesia without sedation did not significantly reduce the incidence of postoperative delirium compared with general anesthesia.
✦ Effect of Intravenous or Intraosseous Calcium vs Saline on Return of Spontaneous Circulation in Adults With Out-of-Hospital Cardiac Arrest
A Randomized Clinical Trial
Administration de Calcium dans l’ACR pré-hospitalier et le retour à une circulation spontanée. Résultats non-en faveur de son utilisation avec arrêt précoce de l’étude pour préjudice.
Importance It is unclear whether administration of calcium has a beneficial effect in patients with cardiac arrest.
Objective To determine whether administration of calcium during out-of-hospital cardiac arrest improves return of spontaneous circulation in adults.
Design, Setting, and Participants This double-blind, placebo-controlled randomized clinical trial included 397 adult patients with out-of-hospital cardiac arrest and was conducted in the Central Denmark Region between January 20, 2020, and April 15, 2021. The last 90-day follow-up was on July 15, 2021.
Interventions The intervention consisted of up to 2 intravenous or intraosseous doses with 5 mmol of calcium chloride (n = 197) or saline (n = 200). The first dose was administered immediately after the first dose of epinephrine.
Main Outcomes and Measures The primary outcome was sustained return of spontaneous circulation. The secondary outcomes included survival and a favorable neurological outcome (modified Rankin Scale score of 0-3) at 30 days and 90 days.
Results Based on a planned interim analysis of 383 patients, the steering committee stopped the trial early due to concerns about harm in the calcium group. Of 397 adult patients randomized, 391 were included in the analyses (193 in the calcium group and 198 in the saline group; mean age, 68 [SD, 14] years; 114 [29%] were female). There was no loss to follow-up. There were 37 patients (19%) in the calcium group who had sustained return of spontaneous circulation compared with 53 patients (27%) in the saline group (risk ratio, 0.72 [95% CI, 0.49 to 1.03]; risk difference, −7.6% [95% CI, −16% to 0.8%]; P = .09). At 30 days, 10 patients (5.2%) in the calcium group and 18 patients (9.1%) in the saline group were alive (risk ratio, 0.57 [95% CI, 0.27 to 1.18]; risk difference, −3.9% [95% CI, −9.4% to 1.3%]; P = .17). A favorable neurological outcome at 30 days was observed in 7 patients (3.6%) in the calcium group and in 15 patients (7.6%) in the saline group (risk ratio, 0.48 [95% CI, 0.20 to 1.12]; risk difference, −4.0% [95% CI, −8.9% to 0.7%]; P = .12). Among the patients with calcium values measured who had return of spontaneous circulation, 26 (74%) in the calcium group and 1 (2%) in the saline group had hypercalcemia.
Conclusions and Relevance Among adults with out-of-hospital cardiac arrest, treatment with intravenous or intraosseous calcium compared with saline did not significantly improve sustained return of spontaneous circulation. These results do not support the administration of calcium during out-of-hospital cardiac arrest in adults.
✦ Effect of Use of a Bougie vs Endotracheal Tube With Stylet on Successful Intubation on the First Attempt Among Critically Ill Patients Undergoing Tracheal Intubation
A Randomized Clinical Trial
Comparaison de deux aides à l’intubation chez les patients de réanimation.
Importance For critically ill adults undergoing emergency tracheal intubation, failure to intubate the trachea on the first attempt occurs in up to 20% of cases and is associated with severe hypoxemia and cardiac arrest. Whether using a tracheal tube introducer (“bougie”) increases the likelihood of successful intubation compared with using an endotracheal tube with stylet remains uncertain.
Objective To determine the effect of use of a bougie vs an endotracheal tube with stylet on successful intubation on the first attempt.
Design, Setting, and Participants The Bougie or Stylet in Patients Undergoing Intubation Emergently (BOUGIE) trial was a multicenter, randomized clinical trial among 1102 critically ill adults undergoing tracheal intubation in 7 emergency departments and 8 intensive care units in the US between April 29, 2019, and February 14, 2021; the date of final follow-up was March 14, 2021.
Interventions Patients were randomly assigned to use of a bougie (n = 556) or use of an endotracheal tube with stylet (n = 546).
Main Outcomes and Measures The primary outcome was successful intubation on the first attempt. The secondary outcome was the incidence of severe hypoxemia, defined as a peripheral oxygen saturation less than 80%.
Results Among 1106 patients randomized, 1102 (99.6%) completed the trial and were included in the primary analysis (median age, 58 years; 41.0% women). Successful intubation on the first attempt occurred in 447 patients (80.4%) in the bougie group and 453 patients (83.0%) in the stylet group (absolute risk difference, −2.6 percentage points [95% CI, −7.3 to 2.2]; P = .27). A total of 58 patients (11.0%) in the bougie group experienced severe hypoxemia, compared with 46 patients (8.8%) in the stylet group (absolute risk difference, 2.2 percentage points [95% CI, −1.6 to 6.0]). Esophageal intubation occurred in 4 patients (0.7%) in the bougie group and 5 patients (0.9%) in the stylet group, pneumothorax was present after intubation in 14 patients (2.5%) in the bougie group and 15 patients (2.7%) in the stylet group, and injury to oral, glottic, or thoracic structures occurred in 0 patients in the bougie group and 3 patients (0.5%) in the stylet group.
Conclusions and Relevance Among critically ill adults undergoing tracheal intubation, use of a bougie did not significantly increase the incidence of successful intubation on the first attempt compared with use of an endotracheal tube with stylet.
✦ Effect of High-Flow Oxygen Therapy vs Conventional Oxygen Therapy on Invasive Mechanical Ventilation and Clinical Recovery in Patients With Severe COVID-19
A Randomized Clinical Trial
Chez les COVID sévères l’Optiflow fait-il mieux que les lunettes d’O2 sur les taux d’IOT & d’amélioration clinique?
Importance The effect of high-flow oxygen therapy vs conventional oxygen therapy has not been established in the setting of severe COVID-19.
Objective To determine the effect of high-flow oxygen therapy through a nasal cannula compared with conventional oxygen therapy on need for endotracheal intubation and clinical recovery in severe COVID-19.
Design, Setting, and Participants Randomized, open-label clinical trial conducted in emergency and intensive care units in 3 hospitals in Colombia. A total of 220 adults with respiratory distress and a ratio of partial pressure of arterial oxygen to fraction of inspired oxygen of less than 200 due to COVID-19 were randomized from August 2020 to January 2021, with last follow-up on February 10, 2021.
Interventions Patients were randomly assigned to receive high-flow oxygen through a nasal cannula (n = 109) or conventional oxygen therapy (n = 111).
Main Outcomes and Measures The co–primary outcomes were need for intubation and time to clinical recovery until day 28 as assessed by a 7-category ordinal scale (range, 1-7, with higher scores indicating a worse condition). Effects of treatments were calculated with a Cox proportional hazards model adjusted for hypoxemia severity, age, and comorbidities.
Results Among 220 randomized patients, 199 were included in the analysis (median age, 60 years; n = 65 women [32.7%]). Intubation occurred in 34 (34.3%) randomized to high-flow oxygen therapy and in 51 (51.0%) randomized to conventional oxygen therapy (hazard ratio, 0.62; 95% CI, 0.39-0.96; P = .03). The median time to clinical recovery within 28 days was 11 (IQR, 9-14) days in patients randomized to high-flow oxygen therapy vs 14 (IQR, 11-19) days in those randomized to conventional oxygen therapy (hazard ratio, 1.39; 95% CI, 1.00-1.92; P = .047). Suspected bacterial pneumonia occurred in 13 patients (13.1%) randomized to high-flow oxygen and in 17 (17.0%) of those randomized to conventional oxygen therapy, while bacteremia was detected in 7 (7.1%) vs 11 (11.0%), respectively.
Conclusions and Relevance Among patients with severe COVID-19, use of high-flow oxygen through a nasal cannula significantly decreased need for mechanical ventilation support and time to clinical recovery compared with conventional low-flow oxygen therapy.
✦ Management of pneumonia in critically ill patients
DOI: https://doi.org/10.1136/bmj-2021-065871
Prise-en-charge de la pneumonie en réa: épidémio, microbio, pathogénicité, traitements & prévention.
Severe pneumonia is associated with high mortality (short and long term), as well as pulmonary and extrapulmonary complications. Appropriate diagnosis and early initiation of adequate antimicrobial treatment for severe pneumonia are crucial in improving survival among critically ill patients. Identifying the underlying causative pathogen is also critical for antimicrobial stewardship.
In this article, we review current knowledge on the management of pneumonia in critically ill patients, including CAP and HAP, focusing on epidemiology, microbial etiology, pathogenesis, treatment, and prevention.
✦ Imposter syndrome; a particular problem for medical students
DOI: https://doi.org/10.1136/bmj.n3048
Le fameux syndrome de l’imposteur, épidémie dont on parle moins mais pourtant…

Les 100% Anesthésie
✦ Identification of myocardial injury using perioperative troponin surveillance in major noncardiac surgery and net benefit over the Revised Cardiac Risk Indexw
DOI: 10.1016/j.bja.2021.10.006
Monitorage de la tropoHS en pré-op & post-op pour dépister les patients les plus à risque de subir un évènement cardiovasculaire ou cérébrovasculaire majeur, ou mortalité: quels cut-off?
Background
Patients with perioperative myocardial injury are at risk of death and major adverse cardiovascular and cerebrovascular events (MACCE). The primary aim of this study was to determine optimal thresholds of preoperative and perioperative changes in high-sensitivity cardiac troponin T (hs-cTnT) to predict MACCE and mortality.
Methods
Prospective, observational, cohort study in patients ≥50 yr of age undergoing elective major noncardiac surgery at seven hospitals in Sweden. The exposures were hs-cTnT measured before and days 0–3 after surgery. Two previously published thresholds for myocardial injury and two thresholds identified using receiver operating characteristic analyses were evaluated using multivariable logistic regression models and externally validated. The weighted comparison net benefit method was applied to determine the additional value of hs-cTnT thresholds when compared with the Revised Cardiac Risk Index (RCRI). The primary outcome was a composite of 30-day all-cause mortality and MACCE.
Results
We included 1291 patients between April 2017 and December 2020. The primary outcome occurred in 124 patients (9.6%). Perioperative increase in hs-cTnT ≥14 ng L−1above preoperative values provided statistically optimal model performance and was associated with the highest risk for the primary outcome (adjusted odds ratio 2.9, 95% confidence interval 1.8–4.7). Validation in an independent, external cohort confirmed these findings. A net benefit over RCRI was demonstrated across a range of clinical thresholds.
Conclusions
Perioperative increases in hsTnT ≥14 ng L−1 above baseline values identifies acute perioperative myocardial injury and provides a net prognostic benefit when added to RCRI for the identification of patients at high risk of death and MACCE.
✦ Anaesthetic depth and delirium after major surgery: a randomised clinical trial
DOI: 10.1016/j.bja.2021.07.021
Un objectif de BIS plus haut (50) en per-op de chirurgie majeure protège-t-il plus nos patients du délirium post-op qu’un objectif plus bas (35)?
Background: Postoperative delirium is a serious complication of surgery associated with prolonged hospitalisation, long-term cognitive decline, and mortality. This study aimed to determine whether targeting bispectral index (BIS) readings of 50 (light anaesthesia) was associated with a lower incidence of POD than targeting BIS readings of 35 (deep anaesthesia).
Methods: This multicentre randomised clinical trial of 655 at-risk patients undergoing major surgery from eight centres in three countries assessed delirium for 5 days postoperatively using the 3 min confusion assessment method (3D-CAM) or CAM-ICU, and cognitive screening using the Mini-Mental State Examination at baseline and discharge and the Abbreviated Mental Test score (AMTS) at 30 days and 1 yr. Patients were assigned to light or deep anaesthesia. The primary outcome was the presence of postoperative delirium on any of the first 5 postoperative days. Secondary outcomes included mortality at 1 yr, cognitive decline at discharge, cognitive impairment at 30 days and 1 yr, unplanned ICU admission, length of stay, and time in electroencephalographic burst suppression.
Results: The incidence of postoperative delirium in the BIS 50 group was 19% and in the BIS 35 group was 28% (odds ratio 0.58 [95% confidence interval: 0.38-0.88]; P=0.010). At 1 yr, those in the BIS 50 group demonstrated significantly better cognitive function than those in the BIS 35 group (9% with AMTS ≤6 vs 20%; P<0.001).
Conclusions: Among patients undergoing major surgery, targeting light anaesthesia reduced the risk of postoperative delirium and cognitive impairment at 1 yr.
✦ Effect of positive end-expiratory pressure on lung injury and haemodynamics during experimental acute respiratory distress syndrome treated with extracorporeal membrane oxygenation and near-apnoeic ventilation
DOI: 10.1016/j.bja.2021.07.031
Comparaison de 3 niveaux de PEP dans le SDRA sous ECMO sur les traumatismes pulmonaires, les échanges gazeux & le retentissement hémodynamique.
Background: Lung rest has been recommended during extracorporeal membrane oxygenation (ECMO) for severe acute respiratory distress syndrome (ARDS). Whether positive end-expiratory pressure (PEEP) confers lung protection during ECMO for severe ARDS is unclear. We compared the effects of three different PEEP levels whilst applying near-apnoeic ventilation in a model of severe ARDS treated with ECMO.
Methods: Acute respiratory distress syndrome was induced in anaesthetised adult male pigs by repeated saline lavage and injurious ventilation for 1.5 h. After ECMO was commenced, the pigs received standardised near-apnoeic ventilation for 24 h to maintain similar driving pressures and were randomly assigned to PEEP of 0, 10, or 20 cm H2O (n=7 per group). Respiratory and haemodynamic data were collected throughout the study. Histological injury was assessed by a pathologist masked to PEEP allocation. Lung oedema was estimated by wet-to-dry-weight ratio.
Results: All pigs developed severe ARDS. Oxygenation on ECMO improved with PEEP of 10 or 20 cm H2O, but did not in pigs allocated to PEEP of 0 cm H2O. Haemodynamic collapse refractory to norepinephrine (n=4) and early death (n=3) occurred after PEEP 20 cm H2O. The severity of lung injury was lowest after PEEP of 10 cm H2O in both dependent and non-dependent lung regions, compared with PEEP of 0 or 20 cm H2O. A higher wet-to-dry-weight ratio, indicating worse lung injury, was observed with PEEP of 0 cm H2O. Histological assessment suggested that lung injury was minimised with PEEP of 10 cm H2O.
Conclusions: During near-apnoeic ventilation and ECMO in experimental severe ARDS, 10 cm H2O PEEP minimised lung injury and improved gas exchange without compromising haemodynamic stability.
✦ Heterogeneous impact of hypotension on organ perfusion and outcomes: a narrative review
DOI: 10.1016/j.bja.2021.06.048
Les effets de l’hypoTA sur la perfusion d’organes & leurs conséquences sous forme de review!
✦ Goal-directed haemodynamic therapy during general anaesthesia for noncardiac surgery: a systematic review and meta-analysis
DOI: 10.1016/j.bja.2021.10.046
Le monitorage de l’hémodynamique en per-op de chirurgie non cardiaque: quels effets en post-op?
Background
During general anaesthesia for noncardiac surgery, there remain knowledge gaps regarding the effect of goal-directed haemodynamic therapy on patient-centred outcomes.
Methods
Included clinical trials investigated goal-directed haemodynamic therapy during general anaesthesia in adults undergoing noncardiac surgery and reported at least one patient-centred postoperative outcome. PubMed and Embase were searched for relevant articles on March 8, 2021. Two investigators performed abstract screening, full-text review, data extraction, and bias assessment. The primary outcomes were mortality and hospital length of stay, whereas 15 postoperative complications were included based on availability. From a main pool of comparable trials, meta-analyses were performed on trials with homogenous outcome definitions. Certainty of evidence was evaluated using Grading of Recommendations, Assessment, Development, and Evaluations (GRADE).
Results
The main pool consisted of 76 trials with intermediate risk of bias for most outcomes. Overall, goal-directed haemodynamic therapy might reduce mortality (odds ratio=0.84; 95% confidence interval [CI], 0.64 to 1.09) and shorten length of stay (mean difference=–0.72 days; 95% CI, –1.10 to –0.35) but with low certainty in the evidence. For both outcomes, larger effects favouring goal-directed haemodynamic therapy were seen in abdominal surgery, very high-risk surgery, and using targets based on preload variation by the respiratory cycle. However, formal tests for subgroup differences were not statistically significant. Goal-directed haemodynamic therapy decreased risk of several postoperative outcomes, but only infectious outcomes and anastomotic leakage reached moderate certainty of evidence.
Conclusions
Goal-directed haemodynamic therapy during general anaesthesia might decrease mortality, hospital length of stay, and several postoperative complications. Only infectious postoperative complications and anastomotic leakage reached moderate certainty in the evidence.
✦ Management of new onset atrial fibrillation in critically unwell adult patients: a systematic review and narrative synthesis
DOI: 10.1016/j.bja.2021.11.016
Revue systématique de la littérature sur la prise-en-charge de la survenue de FA chez les patients instables de réanimation.
Background
New onset atrial fibrillation (NOAF) is the most common arrhythmia affecting critically unwell patients. NOAF can lead to worsening haemodynamic compromise, heart failure, thromboembolic events, and increased mortality. The aim of this systematic review and narrative synthesis is to evaluate the non-pharmacological and pharmacological management strategies for NOAF in critically unwell patients.
Methods
Of 1782 studies, 30 were eligible for inclusion, including 4 RCTs and 26 observational studies. Efficacy of direct current cardioversion, amiodarone, β-antagonists, calcium channel blockers, digoxin, magnesium, and less commonly used agents such as ibutilide are reported.
Results
Cardioversion rates of 48% were reported for direct current cardioversion; however, re-initiation of NOAF was as high as 23.4%. Amiodarone was the most commonly reported intervention with cardioversion rates ranging from 18% to 95.8% followed by β-antagonists with cardioversion rates from 40% to 92.3%. Amiodarone was more effective than diltiazem (odds ratio [OR]=1.91, P=0.32) at cardioversion. Short-acting β-antagonists esmolol and landiolol were more effective compared with diltiazem at cardioversion (OR=3.55, P=0.04) and HR control (OR=3.2, P<0.001).
Conclusion
There was significant variation between studies with regard to the definition of successful cardioversion and heart rate control, making comparisons between studies and interventions difficult. Future RCTs comparing individual anti-arrhythmic agents, in particular magnesium, amiodarone, and β-antagonists, and the role of anticoagulation in critically unwell patients are required. There is also an urgent need for a core outcome dataset for studies of new onset atrial fibrillation to allow comparisons between different anti-arrhythmic strategies.
✦ DALES, Drug Allergy Labels in Elective Surgical patients: a prospective, multicentre cross-sectional study of prevalence, nature and anaesthetists’ approach to management
DOI: https://doi.org/10.1016/j.bja.2021.05.026
En consultation d’anesthésie, il est très fréquent qu’un patient déclare une allergie à un produit administrable en période per et péri opératoire. Nombreux sont les patients ne connaissant pas la ou les réactions les ayant étiqueté « allergique ». Peu d’entre eux sont explorés en ville et l’éviction du potentiel allergène sans documentation semble la solution la plus courante. Néanmoins, le risque est de contre indiquer une classe médicamenteuse au profit d’une alternative moins efficace ou plus sélective, notamment pour les antibiotiques. La consultation d’anesthésie pourrait rattraper ces patients là. Dans cette étude multicentrique de 213 hôpitaux du Royaume Unis, 30% des patients déclarent un risque allergique à un produit d’anesthésie ou antibiotique. Parmi eux, 28% sont considérés à risque de réactions sévères / anaphylaxie de haut grade.
Parmi les molécules incriminées, deux d’entre elles nous intéressent particulièrement, les pénicillines et les opioïdes. Concernant les opioïdes, 916 patients ayant déclaré une réaction allergique étaient suivis. Parmi eux, 37 déclarent des symptômes les classant à haut risque allergique. Sur ces 37, 32 ont reçu un opioïde et aucun n’a souffert d’une allergie. Parmi les 916, 655 recevaient un opioïde dont 76 le traitement spécifique ayant conduit à une réaction allergique. Aucun n’a souffert de risque allergique. Le même groupe avait présenté des résultats concernant les pénicillines.
Ce travail nous éclaire sur le risque moindre des réactions allergiques aux opioïdes par rapport aux déclarations des patients, majoritairement représenté par des intolérances. Il convient toutefois de chercher à préciser ce risque devant la large utilisation de ces molécules en péri anesthésie. Idéalement, il conviendrait de développer des filières de dépistage du risque allergique via une consultation dédiée avec un allergologue avant l’intervention.
Background
We sought to define the prevalence and nature of patient-reported drug allergies, determine their impact on prescribing, and explore drug allergy knowledge and attitudes amongst anaesthetists.
Methods
We performed a prospective cross-sectional study in 213 UK hospitals in 2018. Elective surgical patients were interviewed, with a detailed allergy history taken in those self-reporting drug allergy. Anaesthetists completed a questionnaire concerning perioperative drug allergy.
Results
Of 21 219 patients included, 6214 (29.3 %) (95% confidence interval [CI]: 28.7–29.9) reported drug allergy. Antibiotics, NSAIDs, and opioids were the most frequently implicated agents. Of a total of 8755 reactions, 2462 (28.1%) (95% CI: 29.2–31.1) were categorised as high risk for representing genuine allergy after risk stratification. A history suggestive of chronic spontaneous urticaria significantly increased the risk of reporting drug allergy (odds ratio 2.68; 95% CI: 2.4–3; P<0.01). Of 4756 anaesthetists completing the questionnaire, 1473 (31%) (95% CI: 29.7–32.3) routinely discuss perioperative allergy risk with patients. Prescribing habits in the presence of drug allergy labels differ depending on the implicated agent. Most anaesthetists (4678/4697; 99.6%) (95% CI: 99.4–99.8) prescribe opioids when reactions are consistent with side-effects, although 2269/4697 (48%) (95% CI: 46.9–49.7) would avoid the specific opioid reported.
Conclusions
Almost 30% of UK elective surgical patients report a history of drug allergies, but the majority of reported reactions are likely to be non-allergic reactions. Allergy labels can impact on perioperative prescribing through avoidance of important drugs and use of less effective alternatives. We highlight important knowledge gaps about drug allergy amongst anaesthetists, and the need for improved education around allergy.
✦ 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway
DOI: 10.1097/ALN.0000000000004002
This document is a revision of the “Practice guidelines for management of the difficult airway: A report by the American Society of Anesthesiologists Task Force on Management of the Difficult Airway,” adopted by the ASA in 2012 and published in 2013.1
✦ Carbon Dioxide Changes during High-flow Nasal Oxygenation in Apneic Patients: A Single-center Randomized Controlled Noninferiority Trial
DOI: 10.1097/ALN.0000000000004025
Etude qui vise à mettre en évidence une différence de PaCO2 suite à l’oxygénation apnéique à l’aide de l’OHD avec différents débits d’O2.
Background
Anesthesia studies using high-flow, humidified, heated oxygen delivered via nasal cannulas at flow rates of more than 50 l · min–1 postulated a ventilatory effect because carbon dioxide increased at lower levels as reported earlier. This study investigated the increase of arterial partial pressure of carbon dioxide between different flow rates of 100% oxygen in elective anesthetized and paralyzed surgical adults before intubation.
Methods
After preoxygenation and standardized anesthesia induction with nondepolarizing neuromuscular blockade, all patients received 100% oxygen (via high-flow nasal oxygenation system or circuit of the anesthesia machine), and continuous jaw thrust/laryngoscopy was applied throughout the 15-min period. In this single-center noninferiority trial, 25 patients each, were randomized to five groups: (1) minimal flow: 0.25 l · min–1, endotracheal tube; (2) low flow: 2 l · min–1, continuous jaw thrust; (3) medium flow: 10 l · min–1, continuous jaw thrust; (4) high flow: 70 l · min–1, continuous jaw thrust; and (5) control: 70 l · min–1, continuous laryngoscopy. Immediately after anesthesia induction, the 15-min apnea period started with oxygen delivered according to the randomized flow rate. Serial arterial blood gas analyses were drawn every 2 min. The study was terminated if either oxygen saturation measured by pulse oximetry was less than 92%, transcutaneous carbon dioxide was greater than 100 mmHg, pH was less than 7.1, potassium level was greater than 6 mmol · l–1, or apnea time was 15 min. The primary outcome was the linear rate of mean increase of arterial carbon dioxide during the 15-min apnea period computed from linear regressions.
Results
In total, 125 patients completed the study. Noninferiority with a predefined noninferiority margin of 0.3 mmHg · min–1 could be declared for all treatments with the following mean and 95% CI for the mean differences in the linear rate of arterial partial pressure of carbon dioxide with associated P values regarding noninferiority: high flow versus control, –0.0 mmHg · min–1 (–0.3, 0.3 mmHg · min–1, P = 0.030); medium flow versus control, –0.1 mmHg · min–1 (–0.4, 0.2 mmHg · min–1, P = 0.002); low flow versus control, –0.1 mmHg · min–1 (–0.4, 0.2 mmHg · min–1, P = 0.003); and minimal flow versus control, –0.1 mmHg · min–1 (–0.4, 0.2 mmHg · min–1, P = 0.004).
Conclusions
Widely differing flow rates of humidified 100% oxygen during apnea resulted in comparable increases of arterial partial pressure of carbon dioxide, which does not support an additional ventilatory effect of high-flow nasal oxygenation.
✦ Temporal Transitions in Fibrinolysis after Trauma: Adverse Outcome Is Principally Related to Late Hypofibrinolysis
DOI: 10.1097/ALN.0000000000004036
Relation entre défaillance d’organes post-trauma & la dynamique du système de fibrinolyse pour mieux comprendre l’impact de l’acide tranexamique dans ce contexte.
Background
The relationship between late clinical outcomes after injury and early dynamic changes between fibrinolytic states is not fully understood. The authors hypothesized that temporal transitions in fibrinolysis states using rotational thromboelastometry (ROTEM) would aid stratification of adverse late clinical outcomes and improve understanding of how tranexamic acid modulates the fibrinolytic response and impacts mortality.
Methods
The authors conducted a secondary analysis of previously collected data from trauma patients enrolled into an ongoing prospective cohort study (International Standard Randomised Controlled Trial Number [ISRCTN] 12962642) at a major trauma center in the United Kingdom. ROTEM was performed on admission and at 24 h with patients retrospectively grouped into three fibrinolysis categories: tissue factor–activated ROTEM maximum lysis of less than 5% (low); tissue factor–activated ROTEM maximum lysis of 5 to 15% (normal); or tissue factor–activated ROTEM maximum lysis of more than 15% (high). Primary outcomes were multiorgan dysfunction syndrome and 28-day mortality.
Results
Seven-hundred thirty-one patients were included: 299 (41%) were treated with tranexamic acid and 432 (59%) were untreated. Two different cohorts with low-maximum lysis at 24 h were identified: (1) severe brain injury and (2) admission shock and hemorrhage. Multiple organ dysfunction syndrome was greatest in those with low-maximum lysis on admission and at 24 h, and late mortality was four times higher than in patients who remained normal during the first 24 h (7 of 42 [17%] vs. 9 of 223 [4%]; P = 0.029). Patients that transitioned to or remained in low-maximum lysis had increased odds of organ dysfunction (5.43 [95% CI, 1.43 to 20.61] and 4.85 [95% CI, 1.83 to 12.83], respectively). Tranexamic acid abolished ROTEM hyperfibrinolysis (high) on admission, increased the frequency of persistent low-maximum lysis (67 of 195 [34%]) vs. 8 of 79 [10%]; P = 0.002), and was associated with reduced early mortality (28 of 195 [14%] vs. 23 of 79 [29%]; P = 0.015). No increase in late deaths, regardless of fibrinolysis transition patterns, was observed.
Conclusions
Adverse late outcomes are more closely related to 24-h maximum lysis, irrespective of admission levels. Tranexamic acid alters early fibrinolysis transition patterns, but late mortality in patients with low-maximum lysis at 24 h is not increased.
✦ An advanced double intravenous vasopressor automated system to treat hypotension during spinal anaesthesia for caesarean section
DOI: 10.1097/EJA.0000000000001496
Système de perfusion automatisée de vasopresseurs à l’étude dans le cade de la césarienne sous rachianesthésie pour maintenir une PAS dans les 20% de la normale, prometteur?
BACKGROUND
During spinal anaesthesia for caesarean section, haemodynamic instability may lead to maternal and foetal complications. We developed a novel advanced double intravenous vasopressor automated system (ADIVA) by using a continuous blood pressure and heart rate monitor. Treatment of hypotension was based on three criteria: the drug (phenylephrine or ephedrine) according to the heart rate; the dose of vasopressor determined by the degree of hypotension; a fast or slow bolus of vasopressor administered depending on whether there was a negative or positive gradient of SBP changes, respectively.
OBJECTIVE
The aim of this pilot study was to investigate the feasibility of the ADIVA algorithm.
DESIGN
A prospective pilot study.
SETTING
Single obstetrics and gynaecology centre in Singapore.
PATIENTS
Women undergoing elective caesarean delivery under spinal anaesthesia.
INTERVENTION
Automated administration of ephedrine or phenylephrine based on changes in blood pressure and heart rate (via the ADIVA algorithm) detected on continuous noninvasive haemodynamic monitoring using noninvasive continuous haemodynamic monitor (Nexfin).
MAIN OUTCOME MEASURES
The primary outcome was the incidence of hypotension, defined as SBP less than 80% of baseline. The secondary outcome measures were reactive hypertension, total vasopressor requirement, maternal and neonatal outcomes and system performance.
RESULTS
Forty-five women were recruited. Thirty-one women (69.9%) had at least one reading of hypotension. SBP was within ±20% of the baseline in a mean ± SD of 79.7 ± 17.6% of measurements. Forty-four (97.8%) women required phenylephrine before delivery, while 15 (33.3%) required ephedrine. No rescue medications were required. Three women (6.7%) had nausea and two (4.4%) vomiting. All neonates had APGAR scores of 9 at 5 min.
CONCLUSION
The ADIVA system, with noninvasive continuous haemodynamic monitoring, was able to maintain maternal SBP within ±20% of baseline for the vast majority of the measurements. This system had good maternal and foetal outcomes with minimal intervention from the attending anaesthetist.
✦ Pre-operative fasting in children
A guideline from the European Society of Anaesthesiology and Intensive Care
DOI: 10.1097/EJA.0000000000001599
Nouveautés dans les recos sur le jeûne pré-op en pédiatrie!
Current paediatric anaesthetic fasting guidelines have recommended conservative fasting regimes for many years and have not altered much in the last decades. Recent publications have employed more liberal fasting regimes with no evidence of increased aspiration or regurgitation rates. In this first solely paediatric European Society of Anaesthesiology and Intensive Care (ESAIC) pre-operative fasting guideline, we aim to present aggregated and evidence-based summary recommendations to assist clinicians, healthcare providers, patients and parents.
We identified six main topics for the literature search: studies comparing liberal with conservative regimens; impact of food composition; impact of comorbidity; the use of gastric ultrasound as a clinical tool; validation of gastric ultrasound for gastric content and gastric emptying studies; and early postoperative feeding. The literature search was performed by a professional librarian in collaboration with the ESAIC task force.
Recommendations for reducing clear fluid fasting to 1 h, reducing breast milk fasting to 3 h, and allowing early postoperative feeding were the main results, with GRADE 1C or 1B evidence. The available evidence suggests that gastric ultrasound may be useful for clinical decision-making, and that allowing a ‘light breakfast’ may be well tolerated if the intake is well controlled. More research is needed in these areas as well as evaluation of how specific patient or treatment-related factors influence gastric emptying.
✦ Intra-operative ventilator mechanical power as a predictor of postoperative pulmonary complications in surgical patients
A secondary analysis of a randomised clinical trial
La « puissance mécanique », un nouvel outil pour prévenir les complications respiratoires post-op?
DOI: 10.1097/EJA.0000000000001601
BACKGROUND
Studies in critically ill patients suggest a relationship between mechanical power (an index of the energy delivered by the ventilator, which includes driving pressure, respiratory rate, tidal volume and inspiratory pressure) and complications.
OBJECTIVE
We aimed to assess the association between intra-operative mechanical power and postoperative pulmonary complications (PPCs).
DESIGN
Post hoc analysis of a large randomised clinical trial.
SETTING
University-affiliated academic tertiary hospital in Melbourne, Australia, from February 2015 to February 2019.
PATIENTS
Adult patients undergoing major noncardiothoracic, nonintracranial surgery.
INTERVENTION
Dynamic mechanical power was calculated using the power equation adjusted by the respiratory system compliance (CRS). Multivariable models were used to assess the independent association between mechanical power and outcomes.
MAIN OUTCOME MEASURES
The primary outcome was the incidence of PPCs within the first seven postoperative days. The secondary outcome was the incidence of acute respiratory failure.
RESULTS
We studied 1156 patients (median age [IQR]: 64 [55 to 72] years, 59.5% men). Median mechanical power adjusted by CRS was 0.32 [0.22 to 0.51] (J min−1)/(ml cmH2O−1). A higher mechanical power was also independently associated with increased risk of PPCs [odds ratio (OR 1.34, 95% CI, 1.17 to 1.52); P < 0.001) and acute respiratory failure (OR 1.40, 95% CI, 1.21 to 1.61; P < 0.001).
CONCLUSION
In patients receiving ventilation during major noncardiothoracic, nonintracranial surgery, exposure to a higher mechanical power was independently associated with an increased risk of PPCs and acute respiratory failure.
✦ Intra-operative nociceptive responses and postoperative major complications after gastrointestinal surgery under general anaesthesia
DOI: 10.1097/EJA.0000000000001505
BACKGROUND
Surgical procedures stimulate nociception and induce physiological responses according to the balance between nociception and antinociception. The severity of surgical stimuli is associated with major postoperative complications. Although an intra-operative quantitative index representing surgical invasiveness would be useful for anaesthetic management to predict and prevent major complications, no such index is available.
OBJECTIVES
To identify associations between major complications after gastrointestinal surgery and intra-operative quantitative values from intra-operative nociception monitoring.
DESIGN
A multi-institutional observational study.
SETTING
Two university hospitals.
PATIENTS
Consecutive adult patients undergoing gastrointestinal surgery under general anaesthesia.
MAIN OUTCOME MEASURES
Averaged values of nociceptive response index from start to end of surgery (mean NR index) and risk scores of the Surgical Mortality Probability Model (S-MPM) were calculated. Pre and postoperative serum C-reactive protein (CRP) levels were obtained. After receiver-operating characteristic (ROC) curve analysis, all patients were divided into groups with high and low mean nociceptive response index. Associations between mean nociceptive response index and postoperative major complications, defined as Clavien-Dindo grade at least IIIa, were examined using logistic regression analysis.
RESULTS
ROC curve analysis showed a nociceptive response index cut-off value for major complications of 0.83, and we divided patients into two groups with mean nociceptive response index less than 0.83 and at least 0.83. The incidence of major complications was significantly higher in patients with mean nociceptive response index at least 0.83 (23.1%; n = 346) than in patients with mean nociceptive response index less than 0.83 (7.7%; n = 443; P < 0.001). Multivariate analysis revealed emergency surgery, S-MPM risk score, mean nociceptive response index and postoperative CRP levels as independent risk factors for major complications.
CONCLUSION
Mean nociceptive response index during surgery likely correlates with major complications after gastrointestinal surgery.
✦ Comparison between capnodynamic and thermodilution method for cardiac output monitoring during major abdominal surgery
DOI: 10.1097/EJA.0000000000001566
BACKGROUND
Cardiac output (CO) monitoring is the basis of goal-directed treatment for major abdominal surgery. A capnodynamic method estimating cardiac output (COEPBF) by continuously calculating nonshunted pulmonary blood flow has previously shown good agreement and trending ability when evaluated in mechanically ventilated pigs.
OBJECTIVES
To compare the performance of the capnodynamic method of COmonitoring with transpulmonary thermodilution (COTPTD) in patients undergoing major abdominal surgery.
DESIGN
Prospective, observational, method comparison study. Simultaneous measurements of COEPBF and COTPTD were performed before incision at baseline and before and after increased (+10 cmH2O) positive end-expiratory pressure (PEEP), activation of epidural anaesthesia and intra-operative events of hypovolemia and low CO. The first 25 patients were ventilated with PEEP 5 cmH2O (PEEP5), while in the last 10 patients, lung recruitment followed by individual PEEP adjustment (PEEPadj) was performed before protocol start.
SETTING
Karolinska University Hospital, Stockholm, Sweden.
PATIENTS
In total, 35 patients (>18 years) scheduled for major abdominal surgery with advanced hemodynamic monitoring were included in the study.
MAIN OUTCOME MEASURES AND ANALYSIS
Agreement and trending ability between COEPBF and COTPTD at different clinical moments were analysed with Bland–Altman and four quadrant plots.
RESULTS
In total, 322 paired values, 227 in PEEP5 and 95 in PEEPadj were analysed. Respectively, the mean COEPBF and COTPTD were 4.5 ± 1.0 and 4.8 ± 1.1 in the PEEP5 group and 4.9 ± 1.2 and 5.0 ± 1.0 l min−1 in the PEEPadj group. Mean bias (levels of agreement) and percentage error (PE) were −0.2 (−2.2 to 1.7) l min−1 and 41% for the PEEP5 group and −0.1 (−1.7 to 1.5) l min−1 and 31% in the PEEPadj group. Concordance rates during changes in COEPBF and COTPTD were 92% in the PEEP5 group and 90% in the PEEPadj group.
CONCLUSION
COEPBF provides continuous noninvasive CO estimation with acceptable performance, which improved after lung recruitment and PEEP adjustment, although not interchangeable with COTPTD. This method may become a tool for continuous intra-operative COmonitoring during general anaesthesia in the future.
✦ Neuroprotective effects of intraoperative dexmedetomidine versus saline infusion combined with goal-directed haemodynamic therapy for patients undergoing cranial surgery
A randomised controlled trial
DOI: 10.1097/EJA.0000000000001532
L’utilisation de la dexmedetomidine sous couvert d’un monitorage hémodynamique dans le contexte de chirurgie intracrânienne a-t-elle un effet neuroprotecteur?
BACKGROUND
By inhibiting neuroinflammation dexmedetomidine may be neuroprotective in patients undergoing cranial surgery, but it reduces cardiac output and cerebral blood flow.
OBJECTIVE
To investigate whether intra-operative dexmedetomidine combined with goal-directed haemodynamic therapy (GDHT) has neuroprotective effects in cranial surgery.
DESIGN
A double-blind, single-institution, randomised controlled trial.
SETTING
A single university hospital, from April 2017 to April 2020.
PATIENTS
A total of 160 adults undergoing elective cranial surgery.
INTERVENTION
Infusion of dexmedetomidine (0.5 μg kg−1 h−1) or saline combined with GDHT to optimise stroke volume during surgery.
MAIN OUTCOME MEASURES
The proportion who developed postoperative neurological complications was compared. Postoperative disability was assessed using the Barthel Index at time points between admission and discharge, and also the 30-day modified Rankin Scale (mRS). Postoperative delirium was assessed. The concentration of a peri-operative serum neuroinflammatory mediator, high-mobility group box 1 protein (HMGB1), was compared.
RESULTS
Fewer patients in the dexmedetomidine group developed new postoperative neurological complications (26.3% vs. 43.8%; P = 0.031), but the number of patients developing severe neurological complications was comparable between the two groups (11.3% vs. 20.0%; P = 0.191). In the dexmedetomidine group the Barthel Index reduction [0 (−10 to 0)] was less than that in the control group [−5 (−15 to 0)]; P = 0.023, and there was a more favourable 30-day mRS (P = 0.013) with more patients without postoperative delirium (84.6% vs. 64.2%; P = 0.012). Furthermore, dexmedetomidine induced a significant reduction in peri-operative serum HMGB1 level from the baseline (222.5 ± 408.3 pg ml−1) to the first postoperative day (152.2 ± 280.0 pg ml−1) P = 0.0033. There was no significant change in the control group. The dexmedetomidine group had a lower cardiac index than did the control group (3.0 ± 0.8 vs. 3.4 ± 1.8 l min−1 m−2; P = 0.0482) without lactate accumulation.
CONCLUSIONS
Dexmedetomidine infusion combined with GDHT may mitigate neuroinflammation without undesirable haemodynamic effects during cranial surgery and therefore be neuroprotective.

Les 100% Réanimation
✦ Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock 2021
DOI: 10.1097/CCM.0000000000005337
Chacun s’en fait son propre avis dans le milieu de l’anesthésie et de la réanimation, mais pour ça il faut quand même les avoir lues une bonne fois pour toute !
✦ Sodium chloride or Plasmalyte-148 evaluation in severe diabetic ketoacidosis (SCOPE-DKA): a cluster, crossover, randomized, controlled trial
DOI: 10.1007/s00134-021-06480-5
Plasmalyte vs NaCl 0,9% dans le traitement de l’acidocétose dans un essai de phase 2.
Purpose: To determine whether treatment with Plasmalyte-148 (PL) compared to sodium chloride 0.9% (SC) results in faster resolution of diabetic ketoacidosis (DKA) and whether the acetate in PL potentiates ketosis.
Methods: We conducted a cluster, crossover, open-label, randomized, controlled Phase 2 trial at seven hospitals in adults admitted to intensive care unit (ICU) with severe DKA with hospital randomised to PL or SC as fluid therapy. The primary outcome, DKA resolution, was defined as a change in base excess to ≥ – 3 mEq/L at 48 h.
Results: Ninety-three patients were enrolled with 90 patients included in the modified-intention-to-treat population (PL n = 48, SC n = 42). At 48 h, mean fluid administration was 6798 ± 4850 ml vs 6574 ± 3123 ml, median anion gap 6 mEq/L (IQR 5-7) vs 7 mEq/L (IQR 5-7) and median blood ketones 0.3 mmol/L (IQR 0.1-0.5) vs 0.3 (IQR 0.1-0.5) in the PL and SC groups. DKA resolution at 48 h occurred in 96% (PL) and 86% (SC) of patients; odds ratio 3.93 (95% CI 0.73-21.16, p = 0.111). At 24 h, DKA resolution occurred in 69% (PL) and 36% (SC) of patients; odds ratio 4.24 (95% CI 1.68-10.72, p = 0.002). The median ICU and hospital lengths of stay were 49 h (IQR 23-72) vs 55 h (IQR 41-80) and 81 h (IQR 58-137) vs 98 h (IQR 65-195) in the PL and SC groups.
Conclusion: Plasmalyte-148, compared to sodium chloride 0.9%, may lead to faster resolution of metabolic acidosis in patients with DKA without an increase in ketosis. These findings need confirmation in a large, Phase 3 trial.
✦ High dose coupled plasma filtration and adsorption in septic shock patients. Results of the COMPACT-2: a multicentre, adaptive, randomised clinical trial
DOI: 10.1007/s00134-021-06501-3
Purpose: This study aimed at evaluating the efficacy and safety of high-dose (> 0.2 L/kg of treated plasma per day) coupled plasma filtration-adsorption (CPFA) in treating patients with septic shock.
Methods: Multicentre, randomised, adaptive trial, performed in 12 Italian intensive care units (ICUs). Patients aged 14 or more, admitted to the ICU with septic shock, or had developed it during the stay were eligible. The final outcome was mortality at discharge from the last hospital at which the patient received care.
Results: Between May 2015, and October 2017, 115 patients were randomised. The first interim analysis revealed a number of early deaths, prompting an unplanned analysis. Last hospital mortality was non-significantly higher in the CPFA (55.6%) than in the control group (46.2%, p = 0.35). The 90-day survival curves diverged in favour of the controls early after randomisation and remained separated afterwards (p = 0.100). An unplanned analysis showed higher mortality in CPFA compared to controls among patients without severe renal failure (p = 0.025); a dose-response relationship was observed between treated plasma volume and mortality (p = 0.010).
Conclusion: The COMPACT-2 trial was stopped due to the possible harmful effect of CPFA in patients with septic shock. The harmful effect, if present, was particularly marked in the early phase of septic shock. Patients not requiring renal replacement therapy seemed most exposed to the possible harm, with evidence of a dose-response effect. Until the mechanisms behind these results are fully understood, the use of CPFA for the treatment of patients with septic shock is not recommended.
✦ Individualised versus conventional glucose control in critically-ill patients: the CONTROLING study-a randomized clinical trial
DOI: 10.1007/s00134-021-06526-8
Purpose: Hyperglycaemia is an adaptive response to stress commonly observed in critical illness. Its management remains debated in the intensive care unit (ICU). Individualising hyperglycaemia management, by targeting the patient’s pre-admission usual glycaemia, could improve outcome.
Methods: In a multicentre, randomized, double-blind, parallel-group study, critically-ill adults were considered for inclusion. Patients underwent until ICU discharge either individualised glucose control by targeting the pre-admission usual glycaemia using the glycated haemoglobin A1c level at ICU admission (IC group), or conventional glucose control by maintaining glycaemia below 180 mg/dL (CC group). A non-commercial web application of a dynamic sliding-scale insulin protocol gave to nurses all instructions for glucose control in both groups. The primary outcome was death within 90 days.
Results: Owing to a low likelihood of benefit and evidence of the possibility of harm related to hypoglycaemia, the study was stopped early. 2075 patients were randomized; 1917 received the intervention, 942 in the IC group and 975 in the CC group. Although both groups showed significant differences in terms of glycaemic control, survival probability at 90-day was not significantly different (IC group: 67.2%, 95% CI [64.2%; 70.3%]; CC group: 69.6%, 95% CI [66.7%; 72.5%]). Severe hypoglycaemia (below 40 mg/dL) occurred in 3.9% of patients in the IC group and in 2.5% of patients in the CC group (p = 0.09). A post hoc analysis showed for non-diabetic patients a higher risk of 90-day mortality in the IC group compared to the CC group (HR 1.3, 95% CI [1.05; 1.59], p = 0.018).
Conclusion: Targeting an ICU patient’s pre-admission usual glycaemia using a dynamic sliding-scale insulin protocol did not demonstrate a survival benefit compared to maintaining glycaemia below 180 mg/dL.
✦ Hyperdynamic Left Ventricular Ejection Fraction in ICU Patients With Sepsis
DOI: 10.1097/CCM.0000000000005315
Objectives:
To evaluate the cause and prognosis of hyperdynamic left ventricular ejection fraction in critically ill patients with sepsis.
Design:
Retrospective, single-center cohort study.
Setting:
University Hospital ICU, Birmingham, United Kingdom.
Patients:
ICU patients who received a transthoracic echocardiogram within 7 days of sepsis between April 2016 and December 2019.
Intervention:
None.
Measurements and Main results:
The 90-day mortality rates of normal (55–70%), depressed (< 55%), and hyperdynamic left ventricular ejection fraction (> 70%) were compared. Multivariate logistic regression analysis was performed to determine the association of left ventricular ejection fraction phenotypes with mortality and the association of clinical variables with left ventricular ejection fraction phenotypes. One-thousand fourteen patients met inclusion criteria and were 62 years old (interquartile range, 47–72), with mostly respiratory infections (n = 557; 54.9%). Ninety-day mortality was 32.1% (n = 325). Patients with hyperdynamic left ventricular ejection fraction had a higher mortality than depressed and normal left ventricular ejection fraction cohorts (58.9% [n = 103] vs 34.0% [n = 55] vs 24.7% [n = 167]; p < 0.0001, respectively). After multivariate logistic regression, hyperdynamic left ventricular ejection fraction was independently associated with mortality (odds ratio, 3.90 [2.09–7.40]), whereas depressed left ventricular ejection fraction did not (odds ratio, 0.62 [0.28–1.37]). Systemic vascular resistance was inversely associated with hyperdynamic left ventricular ejection fraction (odds ratio, 0.79 [0.58–0.95]), and age, frailty, and ischemic heart disease were associated with depressed left ventricular ejection fraction.
Conclusions:
Hyperdynamic left ventricular ejection fraction was associated with mortality in septic ICU patients and may reflect unmitigated vasoplegia from sepsis. Depressed left ventricular ejection fraction was not associated with mortality but was associated with cardiovascular disease.
✦ Clinical Benefit of Extubation in Patients on Venoarterial Extracorporeal Membrane Oxygenation
DOI: 10.1097/CCM.0000000000005304
Objectives:
Although patients on venoarterial extracorporeal membrane oxygenation for refractory cardiogenic shock are usually supported with mechanical ventilation, it is not clear whether sedation cessation and extubation might improve outcomes.
Design:
Retrospective cohort study with propensity score overlap weighting analysis.
Setting:
Three ICUs in a 1,500-bed tertiary university hospital.
Patients:
From an overall cohort of 641 patients with venoarterial-extracorporeal membrane oxygenation support, the primary analysis was performed in 344 patients who had been successfully decannulated in order to reduce immortal time bias.
Measurements and Main Results:
Seventy-five patients (22%) were extubated during extracorporeal membrane oxygenation support and were subsequently decannulated alive. Forty-nine percent received noninvasive ventilation, and 25% had emergency reintubation for respiratory, neurologic, or hemodynamic reasons. Higher Simplified Acute Physiology Score II at admission (odds ratio, 0.97; 95% CI [0.95–0.99]; p = 0.008) was associated with a lower probability of extubation, whereas cannulation in cardiac surgery ICU (odds ratio, 3.14; 95% CI [1.21–8.14]; p = 0.018) was associated with an increased probability. Baseline characteristics were well balanced after propensity score overlap weighting. The number of ICU-free days within 30 days of extracorporeal membrane oxygenation decannulation was significantly higher among extubated patients compared with nonextubated patients (22 d [11–26 d] vs 18 d [7–25 d], respectively; p = 0.036). There were no differences in other outcomes including ventilator-associated pneumonia (odds ratio, 0.96; 95% CI [0.51–1.82]; p = 0.90) and all-cause mortality within 30 days of extracorporeal membrane oxygenation decannulation (5% vs 17%; hazard ratio, 0.54; 95% CI [0.19–1.59]; p = 0.27).
As a secondary analysis, outcomes were compared in the overall cohort of 641 venoarterial extracorporeal membrane oxygenation–supported patients. Results were consistent with the primary analysis as extubated patients had a higher number of ICU-free days (18 d [0–24 d] vs 0 d [0–18 d], respectively; < 0.001) and a lower risk of death within 30 days of extracorporeal membrane oxygenation cannulation (hazard ratio, 0.45; 95% CI [0.29–0.71]; p = 0.001).
Conclusions:
Extubation during venoarterial-extracorporeal membrane oxygenation support is safe, feasible, and associated with greater ICU-free days.
✦ Rapid Development and Deployment of an Intensivist-Led Venovenous Extracorporeal Membrane Oxygenation Cannulation Program
DOI: 10.1097/CCM.0000000000005282
Objectives:
To determine the safety and efficacy of a rapidly deployed intensivist-led venovenous extracorporeal membrane oxygenation cannulation program in a preexisting extracorporeal membrane oxygenation program.
Design:
A retrospective observational before-and-after study of 40 patients undergoing percutaneous cannulation for venovenous extracorporeal membrane oxygenation in an established cannulation program by cardiothoracic surgeons versus a rapidly deployed medical intensivist cannulation program.
Setting:
An adult ICU in a tertiary academic medical center in Camden, NJ.
Patients:
Critically ill adult subjects with severe respiratory failure undergoing percutaneous cannulation for venovenous extracorporeal membrane oxygenation.
Interventions:
Percutaneous cannulation for venovenous extracorporeal membrane oxygenation performed by cardiothoracic surgeons compared with cannulations performed by medical intensivists.
Measurements and Main Results:
Venovenous extracorporeal membrane oxygenation cannulation site attempts were retrospectively reviewed. Subject demographics, specialty of physician performing cannulation, type of support, cannulation configuration, cannula size, imaging guidance, success rate, and complications were recorded and summarized. Twenty-two cannulations were performed by three cardiothoracic surgeons in 11 subjects between September 2019 and February 2020. The cannulation program rapidly transitioned to an intensivist-led and performed program in March 2020. Fifty-seven cannulations were performed by eight intensivists in 29 subjects between March 2020 and December 2020. Mean body mass index for subjects did not differ between groups (33.86 vs 35.89; p = 0.775). There was no difference in days on mechanical ventilation prior to cannulation, configuration, cannula size, or discharge condition. There was no difference in success rate of cannulation on first attempt per cannulation site (95.5 vs 96.7; p = 0.483) or major complication rate per cannulation site (4.5 vs 3.5; p = 1).
Conclusions:
There is no difference between success and complication rates of percutaneous venovenous extracorporeal membrane oxygenation canulation when performed by cardiothoracic surgeons versus medical intensivist in an already established extracorporeal membrane oxygenation program. A rapidly deployed cannulation program by intensivists for venovenous extracorporeal membrane oxygenation can be performed with high success and low complication rates.
✦ Intensive care readmissions in the first year after lung transplantation: Incidence, early risk factors and outcome
DOI : 10.1016/j.accpm.2021.100948
Background
Predictive factors of intensive care readmissions after lung transplantation (LT) have not been established. The main objective of this study was to assess early risk factors for ICU readmission during the first year after LT.
Methods
This retrospective, observational, single-centre study included all consecutive patients who underwent LT in our institution between January 2016 and November 2019. Patients who died during the initial hospitalisation in the ICU were excluded. Surgical and medical ICU readmissions were collected during the first year. The results are expressed as medians, interquartile ranges, absolute numbers and percentages. Statistical analyses were performed using the chi-square test, Fisher’s exact test and Mann–Whitney U test as appropriate (p < 0.05 as significance). Multivariate analysis was performed to identify independent risk factors for readmission. The Paris-North-Hospitals Institutional Review Board reviewed and approved the study.
Results
A total of 156 patients were analysed. Eighteen of them (12%) died during the initial ICU hospitalisation. During the first year after LT, ICU readmission was observed for 49/138 (36%) patients. Among these patients, 14/49 (29%) died during the study period. Readmission was mainly related to respiratory failure (35 (71%) patients), infectious diseases (28 (57%) patients), airway complications (11 (22%) patients), and immunologic complications (4 (8%) patients). In the multivariate analysis, ICU readmission was associated with the use of high doses of catecholamines during surgery, and the increased duration of initial ICU stay.
Conclusion
The initial severity of haemodynamic failure and a prolonged postoperative course seem to be key determinants of ICU readmissions after LT.
✦ Fasting does not guarantee empty stomach in the intensive care unit: A prospective ultrasonographic evaluation (The NUTRIGUS study)
DOI: 10.1016/j.accpm.2021.100975
Background
In the intensive care unit (ICU), a fasting period is usually respected to avoid gastric aspiration during airway management procedures. Since there are no recognised guidelines, intensive care physicians balance the aspiration risk with the negative consequences of underfeeding. Our objective was to determine the impact of fasting on gastric emptying in critically ill patients by using gastric ultrasound.
Material and methods
Among the 112 patients that met the inclusion criteria, 100 patients were analysed. Gastric ultrasonography was performed immediately before extubation. Patients with either 1/ an absence of visualised gastric content (qualitative evaluation) or 2/ a gastric volume < 1.5 mll/kg in case of clear fluid gastric content (quantitative evaluation) were classified as having an empty stomach.
Main findings
In our study, twenty-six (26%) patients had a full stomach at the time of extubation. The incidence of full stomach was not significantly different between patients who fasted < 6 h or patients who fasted ≥ 6 h. Among the 57 patients receiving enteral nutrition (EN) within the last 48 h, there was no correlation between the duration of EN interruption and the GAA. The absence of EN was not associated with an empty stomach.
Conclusion
At the time of extubation, the incidence of full stomach was high and not associated with the fasting characteristics (duration/absence of EN). Our results support the notions that fasting before airway management procedures is not a universal paradigm and that gastric ultrasound might represent a useful tool in the tailoring process.
✦ A personalised approach to antibiotic pharmacokinetics and pharmacodynamics in critically ill patients
DOI: 10.1016/j.accpm.2021.100970
Critically ill patients admitted to intensive care unit (ICU) with severe infections, or those who develop nosocomial infections, have poor outcomes with substantial morbidity and mortality. Such patients commonly have suboptimal antibiotic exposures at routinely used antibiotic doses related to an increased volume of distribution and altered clearance due to their underlying altered physiology. Furthermore, the use of extracorporeal devices such as renal replacement therapy and extracorporeal membrane oxygenation in these group of patients also has the potential to alter in vivo drug concentrations. Moreover, ICU patients are likely to be infected with less-susceptible pathogens. Therefore, one potential contributing cause to the poor outcomes observed in critically ill patients may be related to subtherapeutic antibiotic exposures. Newer concepts include the clinician considering optimised dosing based on a blood antibiotic exposure defined by pharmacokinetic modelling and therapeutic drug monitoring, combined with a knowledge of the antibiotic penetration into the site of infection, thereby achieving optimal bacterial killing. Such optimised dosing is likely to improve patient outcomes. The aim of this review is to highlight key aspects of antibiotic pharmacokinetics and pharmacodynamics (PK/PD) in critically ill patients and provide a PK/PD approach to tailor antibiotic dosing to the individual patient.
✦ Gas conditioning during helmet noninvasive ventilation: effect on comfort, gas exchange, inspiratory effort, transpulmonary pressure and patient–ventilator interaction
DOI: 10.1186/s13613-021-00972-9
Background
There is growing interest towards the use of helmet noninvasive ventilation (NIV) for the management of acute hypoxemic respiratory failure. Gas conditioning through heat and moisture exchangers (HME) or heated humidifiers (HHs) is needed during facemask NIV to provide a minimum level of humidity in the inspired gas (15 mg H2O/L). The optimal gas conditioning strategy during helmet NIV remains to be established.
Methods
Twenty patients with acute hypoxemic respiratory failure (PaO2/FiO2 < 300 mmHg) underwent consecutive 1-h periods of helmet NIV (PEEP 12 cmH2O, pressure support 12 cmH2O) with four humidification settings, applied in a random order: double-tube circuit with HHs and temperature set at 34 °C (HH34) and 37 °C (HH37); Y-piece circuit with HME; double-tube circuit with no humidification (NoH). Temperature and humidity of inhaled gas were measured through a capacitive hygrometer. Arterial blood gases, discomfort and dyspnea through visual analog scales (VAS), esophageal pressure swings (ΔPES) and simplified pressure–time product (PTPES), dynamic transpulmonary driving pressure (ΔPL) and asynchrony index were measured in each step.
Results
Median [IqR] absolute humidity, temperature and VAS discomfort were significantly lower during NoH vs. HME, HH34 and HH37: absolute humidity (mgH2O/L) 16 [12–19] vs. 28 [23–31] vs. 28 [24–31] vs. 33 [29–38], p < 0.001; temperature (°C) 29 [28–30] vs. 30 [29–31] vs. 31 [29–32] vs 32. [31–33], p < 0.001; VAS discomfort 4 [2–6] vs. 6 [2–7] vs. 7 [4–8] vs. 8 [4–10], p = 0.03. VAS discomfort increased with higher absolute humidity (p < 0.01) and temperature (p = 0.007). Higher VAS discomfort was associated with increased VAS dyspnea (p = 0.001). Arterial blood gases, respiratory rate, ΔPES, PTPES and ΔPL were similar in all conditions. Overall asynchrony index was similar in all steps, but autotriggering rate was lower during NoH and HME (p = 0.03).
Conclusions
During 1-h sessions of helmet NIV in patients with hypoxemic respiratory failure, a double-tube circuit with no humidification allowed adequate conditioning of inspired gas, optimized comfort and improved patient–ventilator interaction. Use of HHs or HME in this setting resulted in increased discomfort due to excessive heat and humidity in the interface, which was associated with more intense dyspnea.
✦ Diagnosing capillary leak in critically ill patients: development of an innovative scoring instrument for non-invasive detection
DOI: 10.1186/s13613-021-00965-8
Background
The concomitant occurrence of the symptoms intravascular hypovolemia, peripheral edema and hemodynamic instability is typically named Capillary Leak Syndrome (CLS) and often occurs in surgical critical ill patients. However, neither a unitary definition nor standardized diagnostic criteria exist so far. We aimed to investigate common characteristics of this phenomenon with a subsequent scoring system, determining whether CLS contributes to mortality.
Methods
We conducted this single-center, observational, multidisciplinary, prospective trial in two separately run surgical ICUs of a tertiary academic medical center. 200 surgical patients admitted to the ICU and 30 healthy volunteers were included. Patients were clinically diagnosed as CLS or No-CLS group (each N = 100) according to the grade of edema, intravascular hypovolemia, hemodynamic instability, and positive fluid balance by two independent attending physicians with > 10 years of experience in ICU. We performed daily measurements with non-invasive body impedance electrical analysis, ultrasound and analysis of serum biomarkers to generate objective diagnostic criteria. Receiver operating characteristics were used, while we developed machine learning models to increase diagnostic specifications for our scoring model.
Results
The 30-day mortility was increased among CLS patients (12 vs. 1%, P = 0.002), while showing higher SOFA-scores. Extracellular water was increased in patients with CLS with higher echogenicity of subcutaneous tissue [29(24–31) vs. 19(16–21), P < 0.001]. Biomarkers showed characteristic alterations, especially with an increased angiopoietin-2 concentration in CLS [9.9(6.2–17.3) vs. 3.7(2.6–5.6)ng/mL, P < 0.001]. We developed a score using seven parameters (echogenicity, SOFA-score, angiopoietin-2, syndecan-1, ICAM-1, lactate and interleukin-6). A Random Forest prediction model boosted its diagnostic characteristics (AUC 0.963, P < 0.001), while a two-parameter decision tree model showed good specifications (AUC 0.865).
Conclusions
Diagnosis of CLS in critically ill patients is feasible by objective, non-invasive parameters using the CLS-Score. A simplified two-parameter diagnostic approach can enhance clinical utility. CLS contributes to mortality and should, therefore, classified as an independent entity.
✦ Intravenous albumin for the prevention of hemodynamic instability during sustained low-efficiency dialysis: a randomized controlled feasibility trial (The SAFER-SLED Study)
DOI: 10.1186/s13613-021-00962-x
Background
Hemodynamic instability is a frequent complication of sustained low-efficiency dialysis (SLED) treatments in the ICU. Intravenous hyperoncotic albumin may prevent hypotension and facilitate ultrafiltration. In this feasibility trial, we sought to determine if a future trial, powered to evaluate clinically relevant outcomes, is feasible.
Methods
This single-center, blinded, placebo-controlled, randomized feasibility trial included patients with acute kidney injury who started SLED in the ICU. Patients were randomized to receive 25% albumin versus 0.9% saline (control) as 100 mL boluses at the start and midway through SLED, for up to 10 sessions. The recruitment rate and other feasibility outcomes were determined. Secondary exploratory outcomes included ultrafiltration volumes and metrics of hemodynamic instability.
Results
Sixty patients (271 SLED sessions) were recruited over 10 months. Age and severity of illness were similar between study groups. Most had septic shock and required vasopressor support at baseline. Protocol adherence occurred for 244 sessions (90%); no patients were lost to follow-up; no study-related adverse events were observed; open label albumin use was 9% and 15% in the albumin and saline arms, respectively. Ultrafiltration volumes were not significantly different. Compared to the saline group, the albumin group experienced less hemodynamic instability across all definitions assessed including a smaller absolute decrease in systolic blood pressure (mean difference 10.0 mmHg, 95% confidence interval 5.2–14.8); however, there were significant baseline differences in the groups with respect to vasopressor use prior to SLED sessions (80% vs 61% for albumin and saline groups, respectively).
Conclusions
The efficacy of using hyperoncotic albumin to prevent hemodynamic instability in critically ill patients receiving SLED remains unclear. A larger trial to evaluate its impact in this setting, including evaluating clinically relevant outcomes, is feasible.
Du côté des autres spécialités..
✦ Pulmonary Hypertension in the Context of Heart Failure With Preserved Ejection Fraction
DOI : https://doi.org/10.1016/j.chest.2021.08.039
Heart failure with preserved ejection fraction (HFpEF) is the most common form of heart failure and frequently is associated with pulmonary hypertension (PH). HFpEF associated with PH may be difficult to distinguish from precapillary forms of PH, although this distinction is crucial because therapeutic pathways are divergent for the two conditions.
A comprehensive and systematic approach using history, clinical examination, and noninvasive and invasive evaluation with and without provocative testing may be necessary for accurate diagnosis and phenotyping. After diagnosis, HFpEF associated with PH can be subdivided into isolated postcapillary pulmonary hypertension (IpcPH) and combined postcapillary and precapillary pulmonary hypertension (CpcPH) based on the presence or absence of elevated pulmonary vascular resistance. CpcPH portends a worse prognosis than IpcPH. Despite its association with reduced functional capacity and quality of life, heart failure hospitalizations, and higher mortality, therapeutic options focused on PH for HFpEF associated with PH remain limited.
In this review, we aim to provide an updated overview on clinical definitions and hemodynamically characterized phenotypes of PH, pathophysiologic features, therapeutic strategies, and ongoing challenges in this patient population.
✦ Impact of Obesity in Critical Illness
DOI : https://doi.org/10.1016/j.chest.2021.08.001
The prevalence of obesity is rising worldwide. Adipose tissue exerts anatomic and physiological effects with significant implications for critical illness. Changes in respiratory mechanics cause expiratory flow limitation, atelectasis, and V/Q mismatch with resultant hypoxemia. Altered work of breathing and obesity hypoventilation syndrome may cause hypercapnia. Challenging mask ventilation and peri-intubation hypoxemia may complicate intubation. Patients with obesity are at increased risk of ARDS and should receive lung-protective ventilation based on predicted body weight. Increased positive end expiratory pressure (PEEP), coupled with appropriate patient positioning, may overcome the alveolar decruitment and intrinsic PEEP caused by elevated baseline pleural pressure; however, evidence is insufficient regarding the impact of high PEEP strategies on outcomes. Venovenous extracorporeal membrane oxygen-ation may be safely performed in patients with obesity. Fluid management should account for increased prevalence of chronic heart and kidney disease, expanded blood volume, and elevated acute kidney injury risk. Medication pharmacodynamics and pharmacokinetics may be altered by hydrophobic drug distribution to adipose depots and comorbid liver or kidney disease. Obesity is associated with increased risk of VTE and infection; appropriate dosing of prophylactic anticoagulation and early removal of indwelling catheters may decrease these risks. Obesity is associated with improved critical illness survival in some studies. It is unclear whether this reflects a protective effect or limitations inherent to observational research. Obesity is associated with increased risk of intubation and death in SARS-CoV-2 infection. Ongoing molecular studies of adipose tissue may deepen our understanding of how obesity impacts critical illness pathophysiology.





 30 décembre 2021
30 décembre 2021

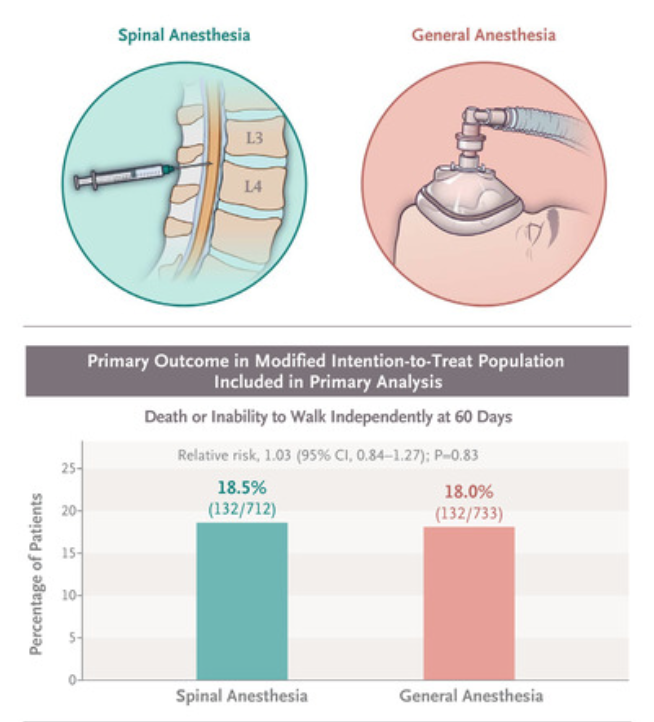
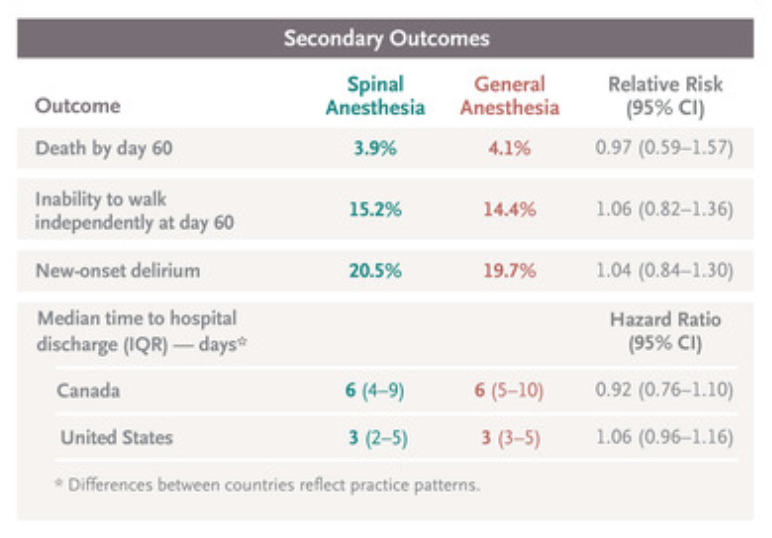




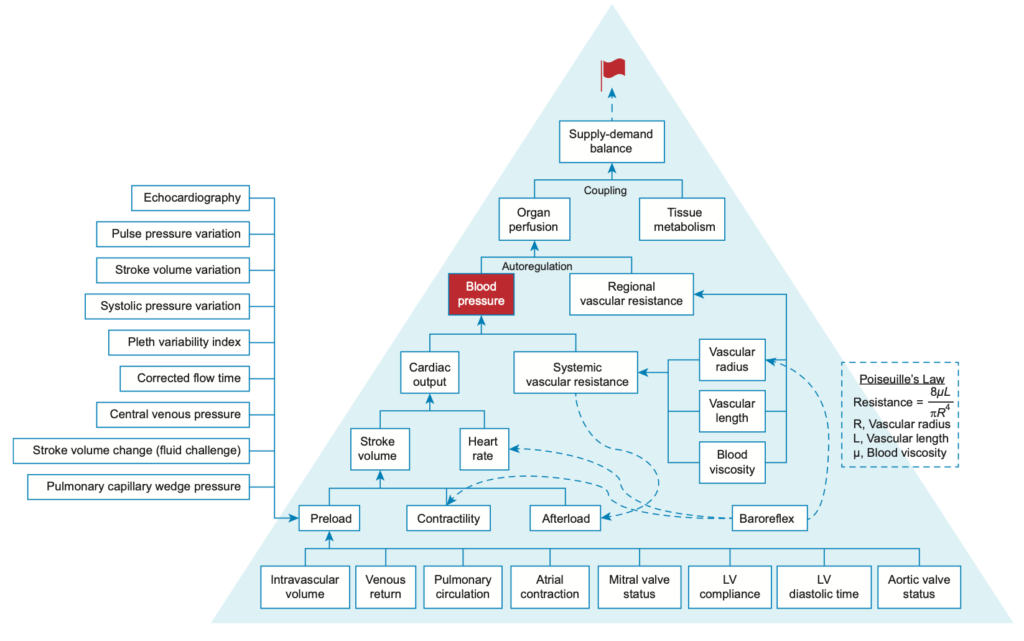





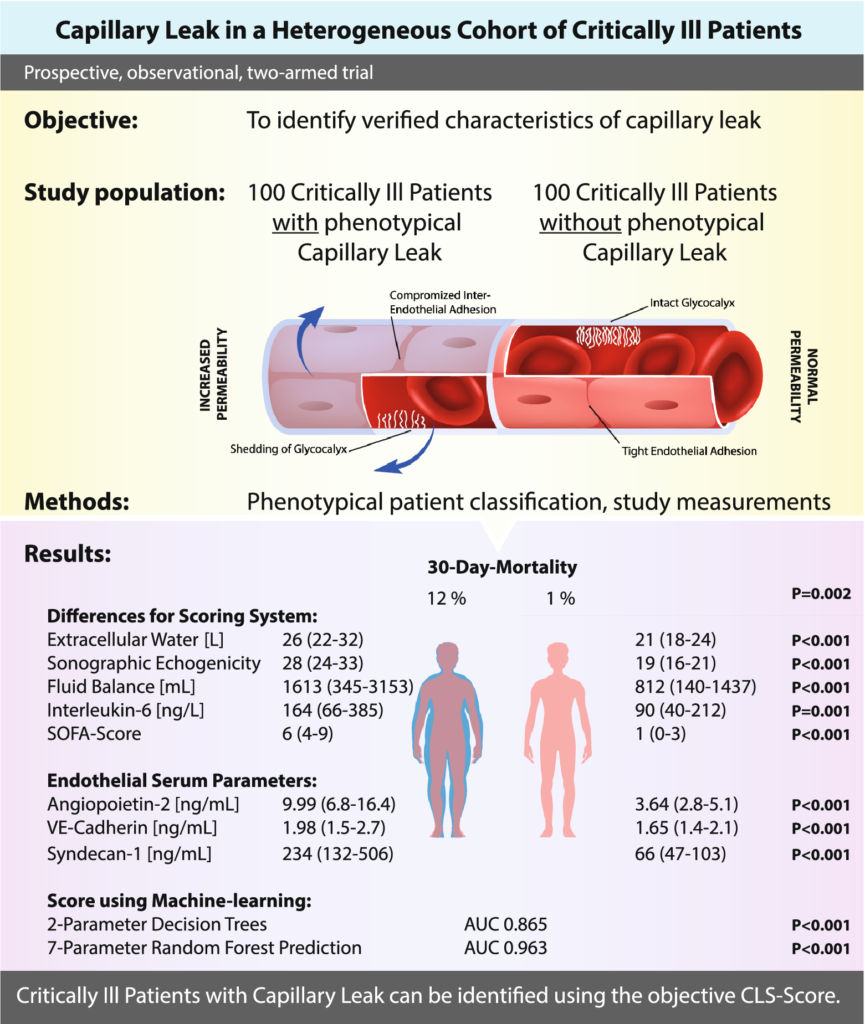

 Étiquettes :
Étiquettes :