LA BIBLIO DU MOIS: Janvier 2021
LA BIBLIO DU MOIS: Janvier 2021
Un début d’année qui commence très fort avec la biblio du mois de Janvier !
Beaucoup de réanimation avec notamment la place de l’ECMO dans l’ACR, les objectifs d’oxygénation dans l’insuffisance respiratoire aiguë, quelques aspects de la prise en charge des patients Covid, et bien d’autres !
Ne manquez pas les bienfaits du thé et du café ☕️ (oui oui, c’est important en anesthésie réanimation!), et prenez quelques minutes pour lire une lettre très émouvante sur la prise de décision conjointe médecins/famille/patient de non admission en réanimation lors de la 1ères vague de COVID.
Enfin, allez jeter un coup d’oeil à la fin de la biblio pour découvrir ou redécouvrir tout ce que vous avez toujours rêvé de savoir sur le coeur droit ! ❤️
Enjoy !
✦ Étude de la Dexaméthasone dans l’hématome sous dural chronique.
Référence : DOI: 10.1056/NEJMoa2020473
–
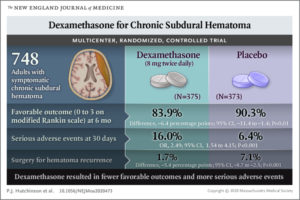
Résumé article :
L’hématome sous dural (HSD) chronique est une pathologie neurologique fréquente en particulier parmi les sujets âgés. L’effet de la Dexamethasone sur le pronostic des patients ayant un HSD chronique n’a pas encore été étudié.
Étude multicentrique randomisée en Grande Bretagne, inclusion de patients avec HDS chronique symptomatique. Les patients étaient assignés avec un ratio 1:1 pour recevoir de la Dexaméthasone per os pendant 15 jours, en débutant à la dose de 8 mg deux fois par jour, ou placebo. La décision d’évacuation chirurgicale de l’hématome était prise par le clinicien.
Le critère de jugement principal était un score de 0 à 3, représentant une évolution favorable, sur l’échelle modifié de Rankin à 6 mois de la randomisation (score de 0 aucun symptôme à 6 la mort).
Résultats : différence significative en faveur du groupe placebo sur le critère de l’évolution favorable à 6 mois. Par ailleurs présence de significativement plus d’effets secondaires indésirables dans le groupe de patients traités par Dexaméthasone.
Conclusion : parmi les adultes avec HSD chronique symptomatique qui ont subi une chirurgie d’évacuation, ceux traités par Dexamethasone ont une évolution plus défavorable, et plus d’effets secondaires indésirables mais moins de reprise chirurgicale.
✦ Rivaroxaban in Patients with Atrial Fibrillation and a Bioprosthetic Mitral Valve
Référence : DOI : 10.1056/NEJMoa2029603
–
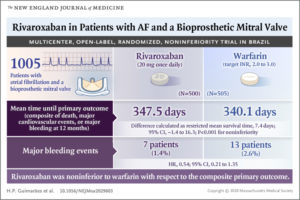
Résumé article :
Les effets du Rivaroxaban chez les patients en FA avec une bioprothèse valvulaire restent incertains.
Étude randomisée comparant le Rivaroxaban 20 mg/ jour à la Warfarin (objectif INR entre 2 et 3) chez patients en FA avec une bioprothèse valvulaire en position mitrale. Critère de jugement principal (CJP) composite : mort, évènement cardiovasculaire majeur (AVC, AIT, embole systémique, thrombose de valve, hospitalisation pour insuffisance cardiaque) ou saignement majeur dans les 12 mois.
Résultats : 1500 patients enrôlés, non infériorité du Rivaroxaban versus la Warfarin en ce qui concerne le CJP. Mortalité d’origine cardiovasculaire et évènements thromboemboliques sont moins fréquents dans le groupe Rivaroxaban (non significatif), incidence des AVC significativement plus faible dans le groupe Rivaroxaban. Saignements majeurs étaient significativement moins fréquents dans le groupe Rivaroxaban. Fréquence des autres effets indésirables étaient similaires dans les deux groupes.
Conclusion : chez les patients en FA avec une bioprothèse mitrale le rivaroxaban est non inférieur à la Warfarin quant au temps moyen avant la survenue d’un évènement majeur entraînant le décès, évènements cardiovasculaires majeurs ou saignements majeurs dans les 12 mois.
✦ Cible haute versus cible basse d’oxygénation dans l’insuffisance respiratoire aigue hypoxémique.
Référence : DOI : 10.1056/NEJMoa2032510
.
Résumé article :
Etude randomisée multicentrique comparant une cible haute (PaO2 90 mmHg) versus une cible basse (PaO2 60 mmHg) chez des patients de soins intensifs admis pour une insuffisance respiratoire aiguë ayant besoin d’oxygène. Hypothèse des auteurs qu’une cible basse permettrait de réduire la mortalité à 90 jours.
Conclusion : absence de différente de mortalité à J90, absence de différence significative de complications au cours du séjour en réanimation.
✦ Dexemetedomidine ou propofol pour la sédation des patients ventilés mécaniquement en réanimation avec sepsis.
Référence : DOI : 10.1056/NEJMoa2024922
.
Résumé article :
Les recommandations recommandent de cibler une sédation légère avec la
dexmethedomidine (DXM) ou le propofol pour les adultes sous ventilation mécanique. Il existe des différences entre les médicaments sédatifs, en termes d’éveil, d’immunité et d’inflammation. Les implications de leur utilisation chez des patients en sepsis sous ventilation mécanique ne sont pas connues.
Étude multicentrique en double aveugle, randomisation des patients ventilés mécaniquement avec sepsis en deux bras : un bras DXM 0,2 à1,5 microgramme/kg/h et un bras propofol 5 à 50 microgramme/kg/min avec des doses ajustées au lit du malade pour atteindre l’objectif de sédation fixé par les cliniciens (échelle de RAS). Le critère de jugement principal est le nombre de jours vécus sans delirium ou comas au cours des 14 jours de l’interventions. CJ secondaires : nombre de jours sans ventilation à 28 jours, mortalité à 90 jours, score cognitif téléphonique ajusté sur l’âge à 6 mois.
Résultats : 432 patients, durée moyenne de récpetion des sédatifs de 3 jours, score RASS moyen à -2, pas de différence entre DXM et propofol dans le nombre de jours vivant sans delirium ou coma, pour le nombre de jours passés sans ventilateur, pour la mortalité à J-90 et pour le score cognitif à 6 mois. Pas de différence concernant les effets secondaires
indésirables.
Conclusion : parmi les patients ventilés mécaniquement avec sepsis dont l’objectif était une sédation légère, les patients sous DXM ont une évolution similaire à ceux sous propofol.
✦ Advanced reperfusion strategies for patients with out-of hospital cardiac arrest and refractory ventricular fibrillation (ARREST): a phase 2, single centre, open-label, randomised controlled trial
Référence : doi.org/10.1016/ S0140-6736(20)32338-2
.
Essai monocentrique de phase 2, comparant chez des patients présentant un arrêt cardio-repiratoire extra-hospitalière avec fibrillation ventriculaire réfractaire, la prise en charge réanimatoire classique à la mise en place d’une ECMO très précoce. Résultats très prometteurs !!
.
Résumé article :
Background – Among patients with out-of-hospital cardiac arrest (OHCA) and ventricular fibrillation, more than half present with refractory ventricular fibrillation unresponsive to initial standard advanced cardiac life support (ACLS) treatment. We did the first randomised clinical trial in the USA of extracorporeal membrane oxygenation (ECMO)- facilitated resuscitation versus standard ACLS treatment in patients with OHCA and refractory ventricular fibrillation.
Methods – For this phase 2, single centre, open-label, adaptive, safety and efficacy randomised clinical trial, we included adults aged 18–75 years presenting to the University of Minnesota Medical Center (MN, USA) with OHCA and refractory ventricular fibrillation, no return of spontaneous circulation after three shocks, automated cardiopulmonary resuscitation with a Lund University Cardiac Arrest System, and estimated transfer time
shorter than 30 min. Patients were randomly assigned to early ECMO-facilitated resuscitation or standard ACLS treatment on hospital arrival by use of a secure schedule generated with permuted blocks of randomly varying block sizes. Allocation concealment was achieved by use of a randomisation schedule that required scratching off an opaque
layer to reveal assignment. The primary outcome was survival to hospital discharge.
Secondary outcomes were safety, survival, and functional assessment at hospital discharge and at 3 months and 6 months after discharge. All analyses were done on an intention-to-treat basis.
Findings – Between Aug 8, 2019, and June 14, 2020, 36 patients were assessed for inclusion.
After exclusion of six patients, 30 were randomly assigned to standard ACLS treatment (n=15) or to early ECMO-facilitated resuscitation (n=15). One patient in the ECMO-facilitated resuscitation group withdrew from the study before discharge. The mean age was 59 years (range 36–73), and 25 (83%) of 30 patients were men. Survival to hospital discharge was observed in one (7%) of 15 patients (95% credible interval 1·6–30·2) in the standard ACLS treatment group versus six (43%) of 14 patients (21·3–67·7) in the early ECMO-facilitated resuscitation group (risk difference 36·2%, 3·7–59·2; posterior probability of ECMO
superiority 0·9861). The study was terminated at the first preplanned interim analysis by the National Heart, Lung, and Blood Institute after unanimous recommendation from the Data Safety Monitoring Board after enrolling 30 patients because the posterior probability of ECMO superiority exceeded the prespecified monitoring boundary. Cumulative 6-month survival was significantly better in the early ECMO group than in the standard ACLS group.
No unanticipated serious adverse events were observed.
Interpretation – Early ECMO-facilitated resuscitation for patients with OHCA and refractory ventricular fibrillation significantly improved survival to hospital discharge compared with standard ACLS treatment.
✦ First-attempt success rate of video laryngoscopy in small infants (VISI): a multicentre, randomised controlled trial
Référence : doi.org/10.1016/S0140-6736(20)32532-0
.
Evaluation de la supériorité de l’intubation par vidéo-laryngoscopie VS laryngoscope direct chez les nourrissons.
Résumé article :
Background – Orotracheal intubation of infants using direct laryngoscopy can be challenging.
We aimed to investigate whether video laryngoscopy with a standard blade done by anaesthesia clinicians improves the first-attempt success rate of orotracheal intubation and reduces the risk of complications when compared with direct laryngoscopy. We hypothesised that the first-attempt success rate would be higher with video laryngoscopy than with direct laryngoscopy.
Methods – In this multicentre, parallel group, randomised controlled trial, we recruited infants without difficult airways abnormalities requiring orotracheal intubation in operating theatres at four quaternary children’s hospitals in the USA and one in Australia. We randomly assigned patients (1:1) to video laryngoscopy or direct laryngoscopy using random permuted blocks of size 2, 4, and 6, and stratified by site and clinician role. Guardians were masked to group assignment. The primary outcome was the proportion of infants with a successful first attempt at orotracheal intubation. Analysis (modified intention-to-treat
[mITT] and per-protocol) used a generalised estimating equation model to account for clustering of patients treated by the same clinician and institution, and adjusted for gestational age, American Society of Anesthesiologists physical status, weight, clinician role, and institution.
Findings – Between June 4, 2018, and Aug 19, 2019, 564 infants were randomly assigned: 282 (50%) to video laryngoscopy and 282 (50%) to direct laryngoscopy. The mean age of infants was 5·5 months (SD 3·3). 274 infants in the video laryngoscopy group and 278 infants in the direct laryngoscopy group were included in the mITT analysis. In the video laryngoscopy group, 254 (93%) infants were successfully intubated on the first attempt compared with 244 (88%) in the direct laryngoscopy group (adjusted absolute risk difference 5·5% [95% CI 0·7 to 10·3]; p=0·024). Severe complications occurred in four (2%) infants in the video laryngoscopy group compared with 15 (5%) in the direct laryngoscopy group (–3·7% [–6·5 to –0·9]; p=0·0087). Fewer oesophageal intubations occurred in the video laryngoscopy group (n=1 [<1%]) compared with in the direct laryngoscopy group (n=7 [3%]; –2·3 [–4·3 to –0·3]; p=0·028).
Interpretation – Among anaesthetised infants, using video laryngoscopy with a standard blade improves the first attempt success rate and reduces complications
✦ Ultra-early tranexamic acid after subarachnoid haemorrhage (ULTRA): a randomised controlled trial
Référence : doi.org/10.1016/S0140-6736(20)32518-6
.
Réduire le risque de resaignement grâce à l’acide tranexamique après une hémorragie sous-arachnoïdienne améliorerait-il la survie à 6 mois des patients ? Il semblerait que non …
.
Résumé article :
Background – In patients with aneurysmal subarachnoid haemorrhage, short-term antifibrinolytic therapy with tranexamic acid has been shown to reduce the risk of rebleeding. However, whether this treatment improves clinical outcome is unclear. We investigated whether ultra-early, short-term treatment with tranexamic acid improves clinical outcome at 6 months.
Methods – In this multicentre prospective, randomised, controlled, open-label trial with masked outcome assessment, adult patients with spontaneous CT-proven subarachnoid haemorrhage in eight treatment centres and 16 referring hospitals in the Netherlands were randomly assigned to treatment with tranexamic acid in addition to care as usual
(tranexamic acid group) or care as usual only (control group). Tranexamic acid was started immediately after diagnosis in the presenting hospital (1 g bolus, followed by continuous infusion of 1 g every 8 h, terminated immediately before aneurysm treatment, or 24 h after start of the medication, whichever came first). The primary endpoint was clinical outcome at 6 months, assessed by the modified Rankin Scale, dichotomised into a good (0–3) or poor (4–6) clinical outcome. Both primary and safety analyses were according to intention to treat.
Findings – Between July 24, 2013, and July 29, 2019, we enrolled 955 patients; 480 patients were randomly assigned to tranexamic acid and 475 patients to the control group. In the intention-to-treat analysis, good clinical outcome was observed in 287 (60%) of 475 patients in the tranexamic acid group, and 300 (64%) of 470 patients in the control group (treatment centre adjusted odds ratio 0·86, 95% CI 0·66–1·12). Rebleeding after randomisation and before aneurysm treatment occurred in 49 (10%) patients in the tranexamic acid and in 66 (14%) patients in the control group (odds ratio 0·71, 95% CI 0·48–1·04). Other serious adverse events were comparable between groups.
Interpretation – In patients with CT-proven subarachnoid haemorrhage, presumably caused by a ruptured aneurysm, ultra-early, short-term tranexamic acid treatment did not improve clinical outcome at 6 months, as measured by the modified Rankin Scale.
✦ Ventilation management and clinical outcomes in invasively ventilated patients with COVID-19 (PRoVENT-COVID): a national, multicentre, observational cohort study
.
Référence: doi.org/10.1016/S2213-2600(20)30459-8
Description et comparaison des paramètres de ventilation invasive des patients traités pour Covid 19 au Pays-Bas.
Résumé article:
Methods – PRoVENT-COVID is a national, multicentre, retrospective observational study done at 18 intensive care units (ICUs) in the Netherlands. Consecutive patients aged at least 18 years were eligible for participation if they had received invasive ventilation for COVID-19 at a participating ICU during the first month of the national outbreak in the Netherlands. The primary outcome was a combination of ventilator variables and parameters over the first 4 calendar days of ventilation: tidal volume, positive end-expiratory pressure (PEEP), respiratory system compliance, and driving pressure. Secondary outcomes included the use of adjunctive treatments for refractory hypoxaemia and ICU complications. Patient-centred outcomes were ventilator-free days at day 28, duration of ventilation, duration of ICU and hospital stay, and mortality.
Findings – Between March 1 and April 1, 2020, 553 patients were included in the study. Median tidal volume was 6·3 mL/kg predicted bodyweight (IQR 5·7–7·1), PEEP was 14·0 cm H2O (IQR 11·0–15·0), and driving pressure was 14·0 cm H2O (11·2–16·0). Median respiratory system compliance was 31·9 mL/cm H2O (26·0–39·9). Of the adjunctive treatments for refractory hypoxaemia, prone positioning was most often used in the first 4 days of ventilation (283 [53%] of 530 patients). The median number of ventilator-free days at day 28 was 0 (IQR 0–15); 186 (35%) of 530 patients had died by day 28. Predictors of 28-day mortality were gender, age, tidal volume, respiratory system compliance, arterial pH, and heart rate on the first day of invasive ventilation.
✦ Efficacy and safety of cefiderocol or best available therapy for the treatment of serious infections caused by carbapenem-resistant Gram-negative bacteria (CREDIBLE-CR): a randomised, open-label, multicentre, pathogen-focused, descriptive, phase 3 trial
.
Référence : doi.org/10.1016/S1473-3099(20)30796-9
.
Efficacité du Cefiderocol dans le traitement des infections à BGN résistantes au carbapénèmases.
.
Résumé article :
✦ Immunopathophysiology of trauma-related acute kidney injury
Une petite review physiopath immuno de l’insuffisance rénale aigue post traumatisme (polytrauma ou autre)
Résumé article : Physical trauma can affect any individual and is globally accountable for more than one in every ten deaths. Although direct severe kidney trauma is relatively infrequent, extrarenal tissue trauma frequently results in the development of acute kidney injury (AKI). Various causes, including haemorrhagic shock, rhabdomyolysis, use of nephrotoxic drugs and infectious complications, can trigger and exacerbate trauma-related
AKI (TRAKI), particularly in the presence of pre-existing or trauma-specific risk factors.
Injured, hypoxic and ischaemic tissues expose the organism to damage-associated and pathogen-associated molecular patterns, and oxidative stress, all of which initiate a complex immunopathophysiological response that results in macrocirculatory and microcirculatory disturbances in the kidney, and functional impairment. The simultaneous activation of components of innate immunity, including leukocytes, coagulation factors and complement
proteins, drives kidney inflammation, glomerular and tubular damage, and breakdown of the blood–urine barrier. This immune response is also an integral part of the intense post- trauma crosstalk between the kidneys, the nervous system and other organs, which aggravates multi-organ dysfunction. Necessary lifesaving procedures used in trauma management might have ambivalent effects as they stabilize injured tissue and organs while simultaneously exacerbating kidney injury. Consequently, only a small number of pathophysiological and immunomodulatory therapeutic targets for TRAKI prevention have been proposed and evaluated.
✦ Safety and 30-days outcomes of tracheostomy for COVID-19: a prospective observational cohort study
.
Référence :doi.org/10.1016/j.bja.2020.08.023
.
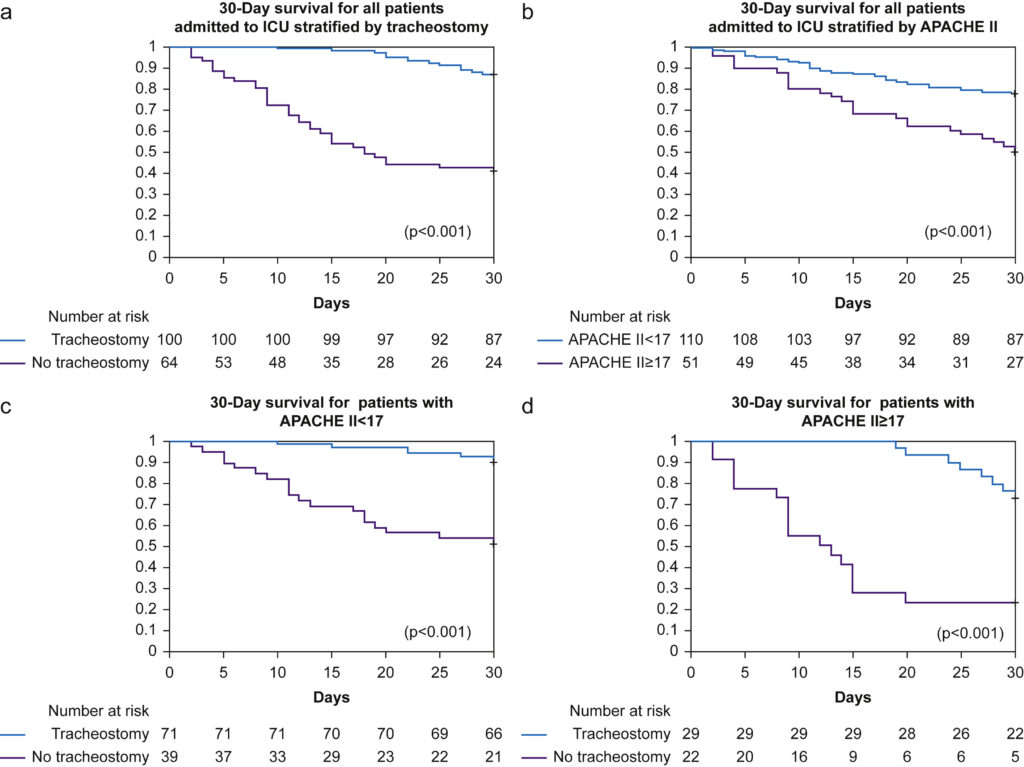
Fig 1Kaplan–Meier plot for 30-day survival from date of intubation. Number at risk detailed below chart. (a) All patients stratified by tracheostomy. (b) All patients stratified by APACHE II score. (c) All patients with APACHE II score<17, stratified by tracheostomy. (d) All patients with APACHE II score ≥17, stratified by tracheostomy. P
.
La trachéostomie chez les Covid 19, c’est safe ou c’est pas safe ?
.
Résumé article :
Background – The role of tracheostomy in coronavirus disease 2019 (COVID-19) is unclear, with several consensus guidelines advising against this practice. We developed both a dedicated airway team and coordinated education programme to facilitate ward management of tracheostomised COVID-19 patients. Here, we report outcomes in the first 100 COVID-19 patients who underwent tracheostomy at our institution.
Methods – This was a prospective observational cohort study of patients confirmed to have COVID-19 who required mechanical ventilation at Queen Elizabeth Hospital, Birmingham, UK. The primary outcome measure was 30-day survival, accounting for severe organ dysfunction (Acute Physiology and Chronic Health [APACHE]-II score>17). Secondary
outcomes included duration of ventilation, ICU stay, and healthcare workers directly involved in tracheostomy care acquiring COVID-19.
Results – A total of 164 patients with COVID-19 were admitted to the ICU between March 9, 2020 and April 21, 2020. A total of 100 patients (mean [standard deviation] age: 55 [12] yr; 29% female) underwent tracheostomy; 64 (age: 57 [14] yr; 25% female) did not undergo tracheostomy. Despite similar APACHE-II scores, 30-day survival was higher in 85/100 (85%) patients after tracheostomy, compared with 27/64 (42%) non tracheostomised patients {relative risk: 3.9 (95% confidence intervals [CI]: 2.3–6.4); P<0.0001}. In patients with APACHE-II scores ≥17, 68/100 (68%) tracheotomised patients survived, compared with 12/64 (19%) non-tracheotomised patients (P<0.001). Tracheostomy within 14 days of intubation was associated with shorter duration of ventilation (mean difference: 6.0 days [95% CI: 3.1–9.0]; P<0.0001) and ICU stay (mean difference: 6.7 days [95% CI: 3.7–9.6]; P<0.0001). No healthcare workers developed COVID-19.
Conclusion – Independent of the severity of critical illness from COVID-19, 30-day survival was higher and ICU stay shorter in patients receiving tracheostomy. Early tracheostomy appears to be safe in COVID-19.
✦ Prone positioning for patients intubated for severe acute respiratory distress syndrome (ARDS) secondary to Covid 19 : a retrospective observational cohort study
Référence : doi.org/10.1016/j.bja.2020.09.042
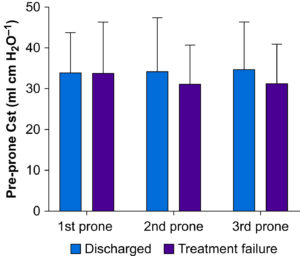
Respiratory system compliance and prone positioning. Using the change in Pao2/Fio2 ratio pre- and post-prone positioning ≥20% as the response criteria, 26 subjects met the criteria in the first prone positioning session (n=36) whereas 13 and 11 subjects responded in the second (n=27) and third (n=20) prone positioning sessions, respectively. Responders’ respiratory system compliance before each prone positioning in the three sessions was similar to non-responders. Cst, compliance of respiratory system.
Résumé article :
Background – The role of repeated prone positioning in intubated subjects with acute respiratory distress syndrome caused by COVID-19 remains unclear.
Exclusion criteria were pregnancy, reintubation, and previous prone positioning at a referring hospital. Patients were followed up until hospital discharge. The primary outcome was oxygenation assessed by partial pressure of oxygen/fraction of inspired oxygen ratio (Pao2/Fio2) ratio. A positive response to proning was defined as an increase in Pao2/Fio2 ratio ≥20%. Treatment failure of prone positioning was defined as death or requirement for extracorporeal membrane oxygenation (ECMO).
subjects who were discharged from hospital were more likely to have an improvement in Pao2/Fio2 ratio ≥20%, compared with those requiring ECMO or who died.
✦ Association between postoperative haemoglobin and myocardial injury after noncardiac surgery: a retrospective cohort analysis
Référence : doi.org/10.1016/j.bja.2020.08.056Résumé article :
✦ Consensus guidelines on perioperative management of malignant hyperthermia suspected or susceptible patients from the European Malignant Hyperthermia groupe
Référence : doi.org/10.1016/j.bja.2020.09.029
Etat des lieux des recommandations de la prise en charge de l’hyperthermie maligne au bloc opératoire, ICI
✦ The PREVENNT randomised, double-blind, controlled trial of preoperative intravenous iron to treat anemia before major abdominal surgery : an independent discussion
Y’a-t-il un intérêt à perfuser du fer en pré-opératoire chez les patients anémiques allant recevoir une chirurgie abdominale ?
Anaemia is a common finding in patients presenting for major elective surgery and is associated with poor outcomes including death and complications. Iron deficiency is the leading cause of perioperative anaemia. Intravenous (i.v.) iron is considered to be an effective and safe treatment for iron deficiency anaemia and is recommended by expert opinion for treatment of preoperative anaemia, although evidence from clinical trials is lacking. The PREVENTT trial was a large multicentre trial investigating the effects of i.v. iron on red cell transfusion, death, complications and quality of life in 487 patients undergoing major abdominal surgery. The principal finding of this multicentre randomised placebo controlled trial was that there was no difference in the co-primary outcomes of blood transfusion or death, or the number of transfusion episodes, within 30 days after surgery, in patients that received preoperative i.v. iron therapy compared to placebo. The major inferential differences in this independent discussion relate to the limitations of the PREVENTT trial and its implications for future practice. Although PREVENTT represents the best evidence available to guide perioperative use of i.v. iron, it is likely that the study was underpowered. In the context of already widespread adoption of preoperative i.v. iron therapy, many clinicians may have felt they lacked equipoise. In light of the PREVENTT study routine use of i.v. iron in patients undergoing elective abdominal surgery cannot be recommended. Further research should define the optimum red cell transfusion strategy for patients undergoing surgery and idenify other surgical groups who may benefit from this intervention.
✦ Outcomes after endoscopic retrograde cholangiopancreatography with general anesthesia versus sedation.
Référence : doi.org/10.1016/j.bja.2020.08.057
Background – We tested the primary hypothesis that use of general anaesthesia vs sedation increases vulnerability to adverse discharge (in-hospital mortality or new discharge to a nursing facility) after endoscopic retrograde cholangiopancreatography (ERCP).
Methods – In this retrospective cohort study, adult patients undergoing ERCP with general anaesthesia or sedation at a tertiary care hospital were included. We calculated adjusted absolute risk differences between patients receiving general anaesthesia vs sedation using provider preference-based instrumental variable analysis. We also used mediation analysis to determine whether intraoperative hypotension during general anaesthesia mediated its effect on adverse discharge.
Results – Among 17 538 patients undergoing ERCP from 2007 through 2018, 16 238 received sedation and 1300 received GA. Rates of adverse discharge were 5.8% ( n=938) after sedation and 16.2% ( n=210) after general anaesthesia. Providers’ adjusted mean predicted probabilities of using general anaesthesia for ERCP ranged from 0.2% to 63.2% of individual caseloads. Utilising provider-related variability in the use of general anaesthesia for instrumental variable analysis resulted in an 8.6% risk increase (95% confidence interval, 4.5–12.6%; P<0.001) in adverse discharge among patients receiving general anaesthesia vs sedation. Intraoperative hypotensive events occurred more often during general anaesthesia and mediated 23.8% (95% confidence interval, 3.9–43.7%: P=0.019) of the primary association.
Conclusions – These results suggest that use of sedation during ERCP facilitates reduced adverse discharge for patients for whom general anaesthesia is not clearly indicated. Intraoperative hypotension during general anaesthesia for ERCP partly mediates the increased vulnerability to adverse discharge.
✦ The effect of immediate postoperative Boussignac CPAP on adverse pulmonaryevents after thoracic surgery
.
Référence : DOI : 10.1097/EJA.0000000000001369
.
BACKGROUND – The effectiveness of prophylactic continuous positive pressure ventilation (CPAP) after thoracic surgery is not clearly established.
OBJECTIVE – The aim of this study was to assess the effectiveness of CPAP immediately after lung resection either by thoracotomy or thoracoscopy in preventing atelectasis and pneumonia.
DESIGN – A multicentre, randomised, controlled, open-label trial. Four large University hospitals at Madrid (Spain) from March 2014 to December 2016. Immunocompetent patients scheduled for lung resection, without previous diagnosis of sleep-apnoea syndrome or severe bullous emphysema. Four hundred and sixty-four patients were assessed, 426 were randomised and 422 were finally analysed. Six hours of continuous CPAP through a Boussignac system versus standard care. Primary outcome: incidence of the composite endpoint ‘atelectasis + pneumonia’. Secondary outcome: incidence of the composite endpoint ‘persistent air leak + pneumothorax’.
RESULTS – The primary outcome occurred in 35 patients (17%) of the CPAP group and in 58 (27%) of the control group [adjusted relative risk (ARR) 0.53, 95% CI 0.30 to 0.93]. The secondary outcome occurred in 33 patients (16%) of the CPAP group and in 29 (14%) of the control group [ARR 0.92, 95% CI 0.51 to 1.65].
CONCLUSION – Prophylactic CPAP decreased the incidence of the composite endpoint ‘postoperative atelectasis + pneumonia’ without increasing the incidence of the endpoint ‘postoperative persistent air leaks + pneumothorax’.
✦ Effects on cerebral blood flow of position changes, hyperoxia, CO2 partial pressure variations and the Valsalva manoeuvre
Référence : DOI : 10.1097/EJA.0000000000001356
BACKGROUND – Maintaining adequate blood pressure to ensure proper cerebral blood flow (CBF) during surgery is challenging. Induced mild hypotension, sitting position or unavoidable intra-operative circumstances such as haemorrhage, added to variations in carbon dioxide and oxygen tensions, may influence perfusion. Several of these circumstances may coincide and it is unclear how these may affect CBF.
OBJECTIVE – To describe the variation in transcranial Doppler and regional cerebral oxygen saturation (rSO2), as a surrogate of CBF, after cardiac preload and gravitational positional changes.
DESIGN – Observational study. Operating room at Hospital Clínic de Barcelona. Ten healthy volunteers, white, both sexes. Measurements were performed in the supine, sitting and standing positions during hyperoxia, hypocapnia and hypercapnia protocols and after a Valsalva manoeuvre.
Cardiac index (CI), haemodynamic and respiratory variables, maximal and mean velocities (Vmax, Vmean) (transcranial Doppler) and rSO2 were acquired. Results were analysed using a generalised estimating equation technique.
RESULTS – CI increases more than 16% after a preload challenge were not accompanied by differences in rSO2 or Vmax − Vmean. With positional changes, Vmean decreased more than 7% (P = 0.042) from the supine to the seated position. Hyperoxia induced a cerebral rSO2 increase more than 6% (P = 0.0001) with decreases in Vmax, Vmean and CI values more than 3% (P = 0.001, 0.022 and 0.001) in the supine and standing position. During hypocapnia, CI rose more than 20% from supine to seated and standing (P = 0.0001) with a 4.5% decrease in cerebral rSO2 (P= 0.001) and a decrease of Vmax − Vmean more than 24% in all positions (P = 0.001). Hypercapnia increased cerebral rSO2 more than 17% (P = 0.001), Vmax − Vmean more than 30% (P = 0.001) with no changes in CI. After a Valsalva manoeuvre, rSO2 decreased more than 3% in the right hemisphere in the upright position (P = 0.001). Vmax − Vmean decreased more than 10% (P = 0.001) with no changes in CI.
CONCLUSION – CBF changes in response to cerebral vasoconstriction and vasodilatation were detected with rSO2 and transcranial Doppler in healthy volunteers during cardiac preload and in different body positions. Acute hypercapnia had a greater effect on recorded brain parameters than hypocapnia.
✦ Approche hémodynamique multivariable pour prédire la réponse au remplissage.
Référence : DOI : 10.1097/EJA.0000000000001289
.
Résumé article :
Le volume d’éjection systolique (VES) résulte de l’interaction entre la fonction du ventricule gauche et de la précharge. Le fluid challenge (test de remplissage) induit une réponse qui dépend du temps, de la fonction cardiaque et des caractéristiques vasculaires et capillaires de l’organisme.
L’objectif de l’étude est de déterminer quel déterminant hémodynamique permet de prédire la réponse à 10 et 30 minutes d’un un test de remplissage.
Étude de cohorte observationnelle multicentrique dans des unités de soins intensives.
Patients : 85 patients de soins critiques avec une insuffisance circulatoire diagnostiquée dans les 48 heures de l’admission.
Intervention : test de remplissage avec 500 ml de Ringer Lactate perfusé en 10 minutes. Une augmentation de 10% de l’index du VES était considéré comme une réponse positive.
Le VES, la pression pulsée, l’élastance arterielle, la différence de pression systolo-dicrotique, l’efficience du cycle cardiaque (ECC) étaient mesurée à 1,2,3,4,5,10,15 et 30 minutes après le début du test de remplissage.
Résultats : la pression pulsée, le changement d’élastance arterielle à 1 minute, le EC et la difference Ps-Pdic à 5 minutes permettaient de classifier correctement répondeurs et non répondeurs à 10 minutes.
LES 100% RÉANIMATION :
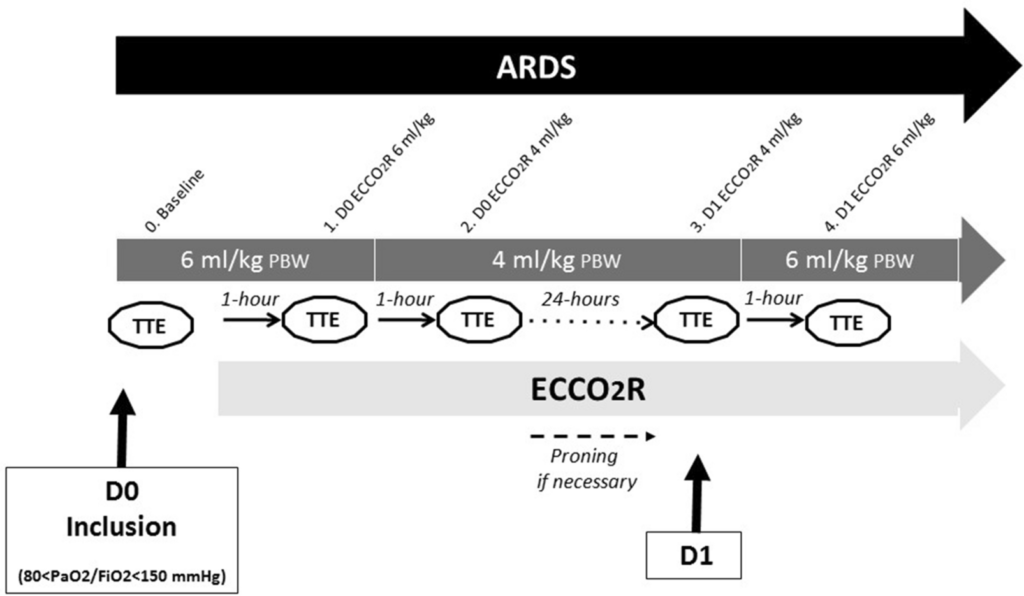
✦ Ultraprotective ventilation allowed by extracorporeal CO2 removal improves the right ventricular function in acute respiratory distress syndrome patients: a quasi- experimental pilot study
.
Référence : doi.org/10.1186/s13613-020-00784-3
.
Study protocol. Transthoracic echocardiography (TTE), extracorporeal CO2 removal (ECCO2R), predictive body weight (PBW), day (D)
.
Un petit article physiopath des ECLS (ici ECCO2R) sur l’hémodynamique
.
Résumé article :
Background – Right ventricular (RV) failure is a common complication in moderate-to-severe acute respiratory distress syndrome (ARDS). RV failure is exacerbated by hypercapnic acidosis and overdistension induced by mechanical ventilation. Veno-venous extracorporeal CO2 removal (ECCO2R) might allow ultraprotective ventilation with lower tidal volume (VT) and plateau pressure (Pplat). This study investigated whether ECCO2R therapy could affect RV function.
Methods – This was a quasi-experimental prospective observational pilot study performed in a French medical ICU. Patients with moderate-to-severe ARDS with PaO2/FiO2 ratio between 80 and 150 mmHg were enrolled. An ultraprotective ventilation strategy was used with VT at 4mL/kg of predicted body weight during the 24 h following the start of a low-flow ECCO2R device. RV function was assessed by transthoracic echocardiography (TTE) during the study protocol.
Results – The efficacy of ECCO2R facilitated an ultraprotective strategy in all 18 patients included. We observed a significant improvement in RV systolic function parameters. Tricuspid annular plane systolic excursion (TAPSE) increased significantly under ultraprotective ventilation compared to baseline (from 22.8 to 25.4 mm; p < 0.05). Systolic excursion velocity (S’ wave) also increased after the 1-day protocol (from 13.8 m/s to 15.1 m/s; p < 0.05). A significant improvement in the aortic velocity time integral (VTIAo) under ultraprotective ventilation settings was observed (p = 0.05). There were no significant differences in the values of systolic pulmonary arterial pressure (sPAP) and RV preload.
Conclusion – Low-flow ECCO2R facilitates an ultraprotective ventilation strategy that would improve RV function in moderate-to-severe ARDS patients. Improvement in RV contractility appears to be mainly due to a decrease in intrathoracic pressure allowed by ultraprotective ventilation, rather than a reduction of PaCO2.
✦ Comparison between regional citrate anticoagulation and heparin for intermittent hemodialysis in ICU patients: a propensity score-matched cohort study
.
Référence : doi.org/10.1186/s13613-021-00803-x
.
Etude rétrospective comparant une anticoagulation citrate calcium à une anticoagulation héparine pour l’hémodialyse intermittente (vu que le CiCa est le gold standard en CVVH/HD/HDF)
.
Résumé article :
Background – Regional citrate anticoagulation (RCA) is the gold standard of anticoagulation for continuous renal replacement therapy but is rarely used for intermittent hemodialysis (IHD) in ICU. Few studies assessed the safety and efficacy of RCA during IHD in ICU; however, no data are available comparing RCA to heparin anticoagulation, which are commonly used for IHD. The aim of this study was to assess the efficacy and safety of RCA compared to heparin anticoagulation during IHD.
Methods – This retrospective single-center cohort study included consecutive ICU patients treated with either heparin anticoagulation (unfractionated or low-molecular-weight heparin) or RCA for IHD from July to September in 2015 and 2017. RCA was performed with citrate infusion according to blood flow and calcium infusion by diffusive influx from dialysate. Using a propensity score analysis, as the primary endpoint we assessed whether RCA improved efficacy, quantified with Kt/V from the ionic dialysance, compared to heparin
anticoagulation. The secondary endpoint was safety. Exploratory analyses were performed on the changes in efficacy and safety between the implementation period (2015) and at long term (2017).
Results – In total, 208 IHD sessions were performed in 56 patients and were compared (124 RCA and 84 heparin coagulation). There was no difference in Kt/V between RCA and heparin (0.95 ± 0.38 vs. 0.89 ± 0.32; p = 0.98). A higher number of circuit clotting (12.9% vs. 2.4%; p = 0.02) and premature interruption resulting from acute high transmembrane pressure (21% vs. 7%; p = 0.02) occurred in the RCA sessions compared to the heparin sessions. In the propensity score-matching analysis, RCA was associated with an increased risk of circuit clotting (absolute differences = 0.10, 95% CI [0.03–0.18]; p = 0.008). There was no difference in efficacy and safety between the two time periods (2015 and 2017).
Conclusion – RCA with calcium infusion by diffusive influx from dialysate for IHD was easy to implement with stable long-term efficacy and safety but did not improve efficacy and could be associated with an increased risk of circuit clotting compared to heparin anticoagulation in non-selected ICU patients. Randomized trials to determine the best anticoagulation for IHD in ICU patients should be conducted in a variety of settings.
✦ Lettre à Denise
.
Référence : https://link.springer.com/article/10.1007/s00134-020-06343-5
.
Résumé article :
Lettre en libre accès, 5 minutes de lecture extrêmement émouvante sur la prise de décision conjointe médecins/patient/famille de non admission en réanimation en mars 2020, lors de la 1 ère vague de la crise COVID. C’est dit avec pudeur, subtilités et avec les mots justes. A lire ICI ✍
✦ Procalcitonin to Reduce Long-Term Infection-associated Adverse Events in Sepsis. A Randomized Trial
.
Référence : DOI: 10.1164/rccm.202004-1201OC
.
La cinétique d’évolution de la PCT permet-elle vraiment
de guider l’arrêt des antibiotiques chez les patients présentant un sepsis notamment par infection des voies aériennes inférieures ? Il semblerait que ce marqueur soit assez fiable !
.
Study primary outcome and the effect of fecal colonization in the intention-to-treat population. (A) Kaplan-Meier curve for primary outcome. The study primary outcome was the rate of infection-associated adverse events for patients allocated to the PCT-guidance group compared with the standard of care after 180 days. Infection-associated adverse events were a composite outcome comprising the advent of any of the following: new case of Clostridioides difficile infection; new case of infection by multidrug-resistant organisms (MDROs); and death due to baseline infection by MDROs or C. difficile. The inset shows the same data on an enlarged y-axis. (B) Odds ratios of reaching or not the primary outcome in dependence of presence or absence of fecal colonization by C. difficile or MDROs by Days 7 and 28. P values of the interaction effect of the arm of treatment by colonization on primary outcome are provided. CI = confidence interval; PCT = procalcitonin.
.
Résumé article :
Rationale: Although early antimicrobial discontinuation guided by procalcitonin (PCT) has shown decreased antibiotic consumption in lower respiratory tract infections, the outcomes in long-term sepsis sequelae remain unclear. Objectives: To investigate if PCT guidance may reduce the incidence of long-term infection-associated adverse events in sepsis. Methods: In this multicenter trial, 266 patients with sepsis (by Sepsis-3 definitions) with lower respiratory tract infections, acute pyelonephritis, or primary bloodstream infection were randomized (1:1) to receive either PCT-guided discontinuation of antimicrobials or standard of care. The discontinuation criterion was ≥80% reduction in PCT levels or any PCT ≤0.5 μg/L at Day 5 or later. The primary outcome was the rate of infection-associated adverse events at Day 180, a composite of the incidence of any new infection by Clostridioides difficile or multidrug-resistant organisms, or any death attributed to baseline C. difficile or multidrug-resistant organism infection. Secondary outcomes included 28-day mortality, length of antibiotic
therapy, and cost of hospitalization. Measurements and Main
Results: The rate of infection-associated adverse events was 7.2% (95% confidence interval [CI], 3.8-13.1%; 9/125) versus 15.3% (95% CI, 10.1-22.4%; 20/131) (hazard ratio, 0.45; 95% CI, 0.20-0.98; P = 0.045); 28-day mortality 15.2% (95% CI, 10-22.5%; 19/125) versus 28.2% (95% CI, 21.2-36.5%; 37/131) (hazard ratio, 0.51; 95% CI, 0.29-0.89; P = 0.02); and median length of antibiotic therapy 5 (range, 5-7) versus 10 (range, 7-15) days (P < 0.001) in the PCT and standard-of-care arms, respectively. The cost of hospitalization was also reduced in the PCT arm.
Conclusions: In sepsis, PCT guidance was effective in reducing infection-associated adverse events, 28-day mortality, and cost of hospitalization.
DU CÔTÉ DES AUTRES SPÉCIALITÉS :
✦ Myocardial Injury in Severe COVID-19 Compared With Non–COVID-19 Acute Respiratory Distress Syndrome
.
reférence : doi.org/10.1161/CIRCULATIONAHA.120.050543
.
.
Background: Knowledge gaps remain in the epidemiology and clinical implications of myocardial injury in coronavirus disease 2019 (COVID-19). We aimed to determine the prevalence and outcomes of myocardial injury in severe COVID-19 compared with acute respiratory distress syndrome (ARDS) unrelated to COVID-19.
Methods: We included intubated patients with COVID-19 from 5 hospitals between March 15 and June 11, 2020, with troponin levels assessed. We compared them with patients from a cohort study of myocardial injury in ARDS and performed survival analysis with primary outcome of in-hospital death associated with myocardial injury. In addition, we performed linear
regression to identify clinical factors associated with myocardial injury in COVID-19.
Results: Of 243 intubated patients with COVID-19, 51% had troponin levels above the upper limit of normal. Chronic kidney disease, lactate, ferritin, and fibrinogen were associated with myocardial injury. Mortality was 22.7% among patients with COVID-19 with troponin under the upper limit of normal and 61.5% for those with troponin levels >10 times the upper limit
of normal (P<0.001). The association of myocardial injury with mortality was not statistically significant after adjusting for age, sex, and multisystem organ dysfunction. Compared with patients with ARDS without COVID-19, patients with COVID-19 were older and had higher creatinine levels and less favorable vital signs. After adjustment, COVID-19–related ARDS was associated with lower odds of myocardial injury compared with non–COVID-19–related ARDS (odds ratio, 0.55 [95% CI, 0.36–0.84]; P=0.005).
Conclusions: Myocardial injury in severe COVID-19 is a function of baseline comorbidities, advanced age, and multisystem organ dysfunction, similar to traditional ARDS. The adverse prognosis of myocardial injury in COVID-19 relates largely to multisystem organ involvement and critical illness.
✦ Ablation Versus Drug Therapy for Atrial Fibrillation in Heart Failure: Results from the CABANA Trial
Référence : doi.org/10.1161/CIRCULATIONAHA.120.050991
Résumé :
Background: In patients with heart failure (HF) and atrial fibrillation (AF), several clinical trials have reported improved outcomes, including freedom from AF recurrence, quality of life (QOL), and survival, with catheter ablation. This report describes the treatment-related outcomes of the AF patients with HF enrolled in the Catheter Ablation vs Antiarrhythmic Drug Therapy for Atrial Fibrillation (CABANA) trial.
Methods: CABANA randomized 2204 patients with AF who were ≥65 years old or <65 with ≥1 risk factor for stroke at 126 sites to ablation with pulmonary vein isolation or drug therapy including rate/rhythm control drugs. Of these, 778 (35%) had NYHA class ≥ II at baseline and form the subject of this report. The CABANA primary endpoint was a composite of death, disabling stroke, serious bleeding, or cardiac arrest.
Results: Of the 778 HF patients enrolled in CABANA, 378 were assigned to ablation and 400 to drug therapy. Ejection fraction (EF) at baseline was available for 571 patients (73%) and 9.3% of these had an EF <40%, while 11.7% had EFs between 40-50%. In the intention-to-treat analysis, the ablation arm had a 36% relative reduction in the primary composite
endpoint (hazard ratio [HR] 0.64; 95% confidence interval [CI], 0.41 to 0.99) and a 43% relative reduction in all-cause mortality (HR 0.57; 95% CI, 0.33 to 0.96) compared to drug therapy alone over a median follow-up of 48.5 months. AF recurrence was decreased with ablation (HR 0.56; 95% CI, 0.42 to 0.74). The adjusted mean difference for the AF Effect on QOL (AFEQT) summary score averaged over the entire 60-month follow-up was 5.0 points favoring the ablation arm (95% CI, 2.5 to 7.4 points), and the Mayo AF-specific Symptom Inventory (MAFSI) frequency score difference was -2.0 points favoring ablation (95% CI, -2.9 to -1.2).
Conclusions: In patients with atrial fibrillation enrolled in CABANA who had clinically diagnosed stable heart failure at trial entry, catheter ablation produced clinically important improvements in survival, freedom from AF recurrence, and quality of life relative to drug therapy. These results, obtained in a cohort most of whom had preserved left ventricular function, require independent trial verification.
✦ Effect of Early Balanced Crystalloids Before ICU Admission on Sepsis Outcomes
.
Référence: doi.org/10.1016/j.chest.2020.08.2068
.
Question récurrente concernant les solutés balancés versus SSI.
Il s’agitd’une analyse secondaire de l’essai SMART ( SMART trial : bénéfice au remplissage parsolutés balancés plutôt que SSI). En se focalisant sur les patients septiques, les auteurs retrouvent une mortalité plus basse (mais NS p=0,07) chez les patients recevant les solutés balancés précocement (aux urgences). Une fois en réa, la mortalité est la même, de quoi alimenter encore les débats (le retard de remplissage “gomme” les effets bénéfiques des
solutés balancés ?). Aux limites de cette étude, s’ajoutent celles de l’étude SMART. (10.1056/NEJMoa1711584. Epub 2018 Feb 27)
.
Background
Studies suggest that using balanced crystalloids (lactated Ringer’s solution or Plasma-Lyte A) rather than saline (0.9% sodium chloride) may improve outcomes for patients with sepsis in the ED and ICU.
Research Question
What is the relative impact on sepsis outcomes of fluid composition during early resuscitation in the ED vs after ICU admission?
Study Design and Methods
We performed a secondary analysis of the Isotonic Solutions and Major Adverse Renal Events Trial (SMART) data set, examining medical ICU patients with a diagnosis of sepsis (n = 1,641). SMART was a cluster-crossover trial comparing balanced crystalloids vs saline among critically ill adults. During the first 7 months of SMART, fluid choice was controlled only in the ICU (“ICU-only period”). In the final 15 months, fluid choice was coordinated between the ED and ICU (“ED and ICU period”). We performed logistic regression modeling for 30-day in-hospital mortality with an interaction term between randomized group (balanced crystalloids vs saline) and study period (ICU-only period vs ED and ICU period).
Results
Three hundred and sixty-seven patients with sepsis were enrolled during the ICU-only period and 1,274 were enrolled during the ED and ICU period. Thirty-day in-hospital mortality occurred in 47 of 142 patients (33.1%) in the balanced crystalloid group vs 74 of 225 patients (32.9%) in the saline group during the ICU-only period (OR, 1.14; 95% CI, 0.70-1.88) and in 170 of 682 patients (24.9%) in the balanced crystalloid group vs 181 of 592 patients (30.6%) in the saline group in the ED and ICU period (OR, 0.68; 95% CI, 0.52-0.89) (P value for interaction, .07), consistent with a beneficial effect of balanced crystalloid primarily in the ED and ICU period.
Interpretation
Among patients with sepsis, the effect of balanced crystalloids vs saline on mortality was greater among patients for whom fluid choice was controlled starting in the ED compared with starting in the ICU.
✦ EFFECT OF ULTRA-SHORT-ACTING β-BLOCKERS ON MORTALITY IN PATIENTS WITH PERSISTENT TACHYCARDIA DESPITE INITIAL RESUSCITATION: A SYSTEMATIC REVIEW AND META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS
.
Référence : doi.org/10.1016/j.chest.2021.01.009
.
Béta Blockers et choc septique “hyperkinétiques”. Il s’agit ici d’une méta analyse sur un sujet d’actualité, à l’aube des inclusions de l’étude Hyper béta
Shock du Pr SLAMA. La mortalité semble abaissée dans ce sous groupe de patients recevant ces BB B1 hyper sélectifs. De quoi faire saliver en attendant les résultats de cet essai multicentrique, randomisé et prospectif ! Attention toutefois aux biais de cette méta analyse (plusieurs BB utilisés)
Background
Historically, β-blockers have been considered to be relatively contraindicated for septic shock because they may cause cardiac suppression. On the other hand, there is an increasing interest in the use of β-blockers for treating septic patients with persistent tachycardia
despite initial resuscitation.
Research question
Do ultra-short-acting β-blockers such as esmolol and landiolol improve mortality in septic patients with persistent tachycardia despite initial resuscitation?
Study design and Methods
This was a systematic review and meta-analysis. We searched MEDLINE, Cochrane Central Register of Controlled Trials, and Embase for RCTs that compared the mortality of patients with sepsis and septic shock treated with esmolol or landiolol. We updated our search on April 20, 2020. Two independent reviewers assessed whether titles and abstracts met the following eligibility criteria: (1) RCT, (2) patients with sepsis and septic shock aged ≥18 years, and (3) treatment with either esmolol/landiolol or placebo/no interventions. Two authors independently extracted selected patient and study characteristics and outcomes. The results of all analyses are presented using random-effect models.
Results
Seven RCTs with a pooled sample size of 613 patients were included. Of these, six RCTs with 572 patients reported 28-day mortality. Esmolol or landiolol use in patients with sepsis and septic shock was significantly associated with lower 28-day mortality (risk ratio, 0.68; 95% CI,
0.54–0.85; P < .001). Unimportant heterogeneity was observed (I2 = 31%). The absolute risk reduction and number of patients to be treated to prevent one death were 18.2% and 5.5, respectively.
Interpretation
The use of ultra-short-acting β-blockers such as esmolol and landiolol in septic patients with persistent tachycardia despite initial resuscitation was associated with significantly lower 28- day mortality.
✦ Green Tea and Coffee Consumption and All-Cause Mortality Among Persons With and Without Stroke or Myocardial Infarction
.
Référence : doi.org/10.1161/STROKEAHA.120.032273
.
Les bienfaits cardiovasculaires du thé vert et du café ☕️🍵
.
Background and Purpose:
The effect of green tea and coffee consumption on mortality among cardiovascular diseases survivors is unknown. We examined the association between green tea and coffee consumption and mortality among persons with and without stroke or myocardial infarction (MI).
Methods:
In the Japan Collaborative Cohort Study, 46 213 participants (478 stroke survivors, 1214 MI survivors, and 44 521 persons without a history of stroke or MI), aged 40 to 79 years at baseline (1988–1990), completed a lifestyle, diet, and medical history questionnaire and were followed up regarding mortality until 2009. The Cox proportional hazard model was used to calculate the multivariable hazard ratios with 95% CIs of all-cause mortality after adjusting for potential confounding factors.
Results:
During the 18.5-year median follow-up period, 9253 cases were documented. Green tea consumption was inversely associated with all-cause mortality among stroke or MI survivors; the multivariable hazard ratios (95% CIs) for stroke survivors were 0.73 (0.42–1.27) for 1 to 6 cups/wk, 0.65 (0.36–1.15) for 1 to 2 cups/d, 0.56 (0.34–0.92) for 3 to 4 cups/d, 0.52 (0.31–0.86) for 5 to 6 cups/d, and 0.38 (0.20–0.71) for ≥7 cups/d, compared with nondrinkers. A similar inverse association was observed for MI survivors, but not evident for those without a history of stroke or MI. Coffee consumption was inversely associated with all-cause mortality in persons without a history of stroke or MI; the multivariable hazard ratios (95% CIs) were 0.86 (0.82–0.91) for 1 to 6 cups/wk, 0.86 (0.80–0.92) for 1 cup/d, and
0.82 (0.77–0.89) for ≥2 cups/d, compared with nondrinkers. The corresponding hazard ratio (95% CIs) for MI survivors were 0.69 (0.53–0.91), 0.78 (0.55–1.10), and 0.61 (0.41–0.90). No such association was observed for stroke survivors.
Conclusions:
Green tea consumption can be beneficial in improving the prognosis for stroke or MI survivors, whereas coffee consumption can also be so for persons without a history of stroke or MI as well as MI survivors.
✦ Prognosis of Intracerebral Hemorrhage Related to Antithrombotic Use
.
Référence : doi/10.1161/STROKEAHA.120.030930
.
Moins bon pronostic des AVC hémorragiques sous anti-agrégants plaquettaires
.
Background and Purpose:
To date, large studies comparing mortality and functional outcome of intracerebral hemorrhage (ICH) during oral anticoagulant (OAC), antiplatelet, and nonantithrombotic use are few and show discrepant results.
Methods:
We used data on 13 291 patients with ICH registered in Riksstroke between 2012 and 2016 to compare 90-day mortality and functional outcome following OAC-related ICH (n=2300), antiplatelet-related ICH (n=3637), and nonantithrombotic ICH (n=7354). Univariable and multivariable Cox regression analyses, with adjustment for relevant confounders, were used
to compare 90-day mortality. Early (≤24 hours and 1–7 days) and late (8–90 days) mortality was also studied in subgroup analyses. Univariable and multivariable 90-day functional outcome, based on self-reported modified Rankin Scale, was determined using logistic regression.
Results:
Patients with antithrombotic treatment were more often prestroke dependent, older, and had a larger comorbidity burden compared with patients without antithrombotic treatment. At 90 days, antiplatelet and OAC were associated with an increased death rate in multivariable analysis (antiplatelet ICH: hazard ratio, 1.23 [95% CI, 1.14–1.33]; OAC ICH:
hazard ratio, 1.40 [95% CI, 1.26–1.57]) compared with nonantithrombotic ICH (reference). OAC ICH and antiplatelet ICH were associated with higher risk of early mortality (≤24 hours: OAC ICH: hazard ratio, 1.93 [95% CI, 1.57–2.38]; antiplatelet ICH: hazard ratio, 1.32 [95% CI,
1.13–1.54]). In multivariable analysis, the odds ratios for the association of antiplatelet and OAC treatment on functional dependency (modified Rankin Scale score, 3–5) at 90 days were nonsignificant (antiplatelet: odds ratio, 1.07 [95% CI, 0.92–1.24]; OAC: odds ratio, 0.96 [95% CI, 0.76–1.22]).
Conclusions: In this large observational study, we found that 90-day mortality outcome was worse not only in OAC ICH but also in antiplatelet ICH, compared with patients with nonantithrombotic ICH. Antiplatelet ICH is common and is a serious condition with poor clinical outcome.
Further studies are, therefore, warranted in determining the appropriate clinical management of these patients.
✦ Statins After Ischemic Stroke in the Oldest
.
Référence: doi/10.1161/STROKEAHA.120.030755
.
Intérêt des statines post-AVC ischémique : Oui mais pas
trop tôt !
.
Background and Purpose:
Statins are frequently initiated in patients aged 80 years and older after an ischemic stroke, even though evidence on prevention of recurrent cardiovascular disease is scarce. In this study, we seek evidence for statin prescription in the oldest old.
Methods:
We performed a retrospective cohort study in patients aged 65 years and older hospitalized for a first ischemic stroke between 1999 and 2016 without statin prescriptions in the year before hospitalization using the Clinical Practice Research Datalink. The age group 65 to 80 years was included to compare our results to current evidence on statin efficacy. The primary outcome was a composite of recurrent stroke, myocardial infarction, and
cardiovascular mortality. The secondary outcome was all-cause mortality. A time-varying Cox model was used to account for statin prescription over time. We compared at least 2 years of statin prescription time with untreated and <2 years of prescription time. Analyses were adjusted for potential confounders. The number needed to treat was calculated based on the adjusted hazard ratios and corrected for deaths during the first 2 years of follow-up.
Results:
Five thousand nine hundred ten patients, aged 65 years and older were included, of whom 3157 were 80 years and older. Two years of statin prescription in patients aged 80 years and older resulted in both a lower risk of the composite end point (adjusted hazard ratio, 0.80 [95% CI, 0.62–1.02]) and all-cause mortality (adjusted hazard ratio, 0.67 [95% CI, 0.57–0.80]). After correction for the mortality of 23.9% of the patients during the first 2 years, the number needed to treat was 64 for the primary outcome during a median follow-up of 3.9 years and 19 for all-cause mortality.
Conclusions:
Statins initiated in patients aged 80 and older, discharged home after hospitalization for an ischemic stroke are associated with a reduction in cardiovascular events.
✦ Impact of Statins on Hematoma, Edema, Seizures, Vascular Events, and Functional Recovery After Intracerebral Hemorrhage
.
Référence: doi/10.1161/STROKEAHA.120.029345
.
Background and Purpose:
The impact of statins on hematoma characteristics, perihemorrhagic edema (PHE), cardiovascular events, seizures, and functional recovery in patients with intracerebral hemorrhage (ICH) is insufficiently studied.
Methods:
Patients with ICH of the prospective UKER-ICH (Universitätsklinikum Erlangen Cohort of Patients With Spontaneous Intracerebral Hemorrhage) study (URL: https://www.clinicaltrials.gov; Unique identifier NCT03183167) were analyzed by multivariable regression modeling and propensity score matching, and PHE volumes were volumetrically assessed. Outcomes comprised hematoma characteristics, the impact of continuation, discontinuation, and initiation of statins on peak PHE extent, and the influence of statin treatment on the occurrence of seizures, cardiovascular adverse events, and functional recovery after ICH.
Results:
A total of 1275 patients with ICH with information on statin treatment were analyzed. Statin treatment on hospital admission (21.7%) was associated with higher rates of lobar versus nonlobar ICH (odds ratio, 1.57 [1.03–2.40]; P=0.038). Initiation of statins after ICH was associated with increased peak PHE (β=0.12, SE=0.06, P=0.008), whereas continuation versus discontinuation of prior statin treatment was not significantly associated with edema formation (P>0.10). There were no significant differences in the incidence of remote symptomatic seizures according to statin exposure during follow-up (statins: 11.5% versus no statins: 7.8%, subdistribution hazard ratio: 1.15 [0.80–1.66]; P=0.512). Patients on statins revealed less cardiovascular adverse events and more frequently functional recovery after
12 months (functional recovery: 57.7% versus 45.0%, odds ratio 1.67 [1.09–2.56]; P=0.019).
Conclusions:
Among statin users, lobar ICH occurs more frequently as compared with nonstatin users. While continuation of prior statin treatment appears to be safe regarding PHE formation, the initiation of statins during the first days after ICH may increase PHE extent. However, statins should be initiated thereafter (eg, at hospital discharge) to prevent cardiovascular events and potentially improve functional recovery.
✦ Impact of Baseline Characteristics on Future Episodes of Bloodstream Infections: Multistate Model in Septic Patients With Bloodstream Infections
.
Référence : doi.org/10.1093/cid/ciz1206
.
Les facteurs de risque de résistance bactérienne sont connues pour une 1ère infection. Ici, les auteurs ont fait une étude observationelle sur l’évolution des germes (+ résistances) retrouvées sur les infections suivantes et étudient les facteurs de risques associés à ces transitions de germes.
.
Background
Looking only at the index infection, studies have described risk factors for infections caused by resistant bacteria. We hypothesized that septic patients with bloodstream infections may transition across states characterized by different microbiology and that their trajectory is not uniform. We also hypothesized that baseline risk factors may influence subsequent blood culture results.
Methods
All adult septic patients with positive blood cultures over a 7-year period were included in the study. Baseline risk factors were recorded. We followed all survivors longitudinally and recorded subsequent blood culture results. We separated states into bacteremia caused by gram-positive cocci, susceptible gram-negative bacilli (sGNB), resistant GNB (rGNB), and Candida spp. Detrimental transitions were considered when transitioning to a culture with a higher mortality risk (rGNB and Candida spp.). A multistate Markov-like model was used to determine risk factors associated with detrimental transitions.
Results
A total of 990 patients survived and experienced at least 1 transition, with a total of 4282 transitions. Inappropriate antibiotics, previous antibiotic exposure, and index bloodstream infection caused by either rGNB or Candida spp. were associated with detrimental transitions. Double antibiotic therapy (beta-lactam plus either an aminoglycoside or a fluoroquinolone) protected against detrimental transitions.
Conclusion
Baseline characteristics that include prescribed antibiotics can identify patients at risk for subsequent bloodstream infections caused by resistant bacteria. By altering the initial treatment, we could potentially influence future bacteremic states.
ARCHIVES:
Retour sur un article déjà paru depuis quelques temps mais qui remet
les idées en place !
Le rôle du retour veineux en soins critiques et dans les états de choc. Partie 1
physiologie.
.
DOI : 10.1097/CCM.0b013e3182772ab6
.
Critical care medicine
Tout ce que vous avez toujours rêvé de savoir (et de comprendre) sur le cœur
droit ! Relations entre Pression systémique moyenne, Pression dans l’oreillette droite, résistance vasculaire systémique et retour veineux… Petit bonus à la fin pour comprendre comment un remplissage vasculaire permet de majorer le débit cardiaque. Poiseuille, Starling, graphiques tout y est.





 18 février 2021
18 février 2021